Commentary
How to stoke an epidemic
Prevalence, Infectivity and Contact Rate are being ignored

A pedestrian walks by a closed sign on the door of a restaurant on March 17, 2020 in San Francisco (Photo by Justin Sullivan/Getty Images)

Gabriel Rotello.
As we watch the disastrous results of reopening and the surge in new infections, I keep thinking that we’re running a giant epidemiological experiment designed to illustrate how to make an epidemic as catastrophic as possible.
In an epidemiological nutshell, the resurgence is happening because we are largely ignoring the three fundamental factors that determine whether an epidemic grows or shrinks, namely Prevalence, Infectivity and Contact Rate. If you really want to bring an infectious epidemic like Covid-19 under control, you better try to address all three.
Prevalence
Prevalence is the percentage of the population that is infectious at any given time.
It’s important because, other things being equal, you will have a lot more transmission in a population where 1 in 10 people are infectious than in a population where only 1 in 10,000 are. The reason why epidemics always begin slowly is because at the beginning of all epidemics, prevalence is inevitably low. As more people get infected, increasing prevalence becomes like a snowball rolling downhill.
Infectivity
Infectivity is the statistical likelihood that a particular pathogen will actually be transmitted when an infectious person and a susceptible person come together.
Different diseases have different levels of infectivity. For example, the infectivity of measles and smallpox is incredibly high while the infectivity of most sexually transmitted diseases (like HIV) is so low you have to exchange significant bodily fluids to achieve transmission. Covid-19 is relatively high, though not as high as measles. Infectivity is obviously important because the more infective a pathogen, the easier and faster it will spread.
Contact Rate
Contact Rate is the rate at which infectious people come into contact with susceptible people in a given population.
It’s essentially the river upon which human-to-human disease transmission flows. The reason for its importance is pretty self-evident.
In a crowded city where people might come into contact with thousands in a single day, diseases have much more opportunity to spread than in a rural area where people might only come into contact with a handful of others.
Because Prevalence, Infectivity and Contact Rate are so important, they form the basis for the three main strategies we use to try to combat epidemics.
The main way to address prevalence (short of a cure or a permanent lockdown) is through testing, contact tracing and quarantine.
The purpose of these prevalence-based strategies is to find infectious people and temporarily remove them from the population, thereby reducing prevalence within that population.

The main ways to address infectivity (at least for respiratory diseases like Covid-19) are by wearing masks, washing hands, staying six feet apart, meeting outdoors rather than indoors, and so on. The idea behind these infectivity-based strategies is to reduce the chance of transmission when infectious people and susceptible people do come together.
This, by the way, is also the idea behind condoms to prevent HIV transmission, and also the more recent strategies for HIV prevention like PrEP, PEP and Treatment as Prevention.
All of these are ways to reduce infectivity per contact.
And finally, we reduce the contact rate itself by keeping potentially infectious and susceptible people apart. That’s why we had the shut-down. Contact rate is so critical that in the case of Covid-19, governments all over the world decided it was worth trashing their economies to bring the contact rate down.
It’s a blunt and painful instrument, but it’s vital if things are spiraling out of control.
So what does all this have to do with the big reopening disaster that’s happening now?
Think of it this way. By re-opening, we are not directly addressing or changing prevalence or infectivity. What we’re doing is increasing the contact rate.
Now you might think that this would automatically increase transmission, but not necessarily, at least if you do it right. That’s because prevalence, infectivity and contact rate work together synergistically, kind of like a seesaw. If one of these factors increases but the other two decrease, things might balance out and you might have a chance of keeping transmission from spiraling out of control.
For example, imagine that you increase the contact rate by reopening the economy. But at the same time, you reduce prevalence by aggressively testing and isolating infective people. And you also reduce infectivity by making sure everyone wears masks, observes the six-feet rule, gathers outdoors rather than indoors and so on.
In that case, the decreases in both prevalence and infectivity might balance the increase in the contact rate and you might avoid a resurgence.
True, it’s hard to balance this seesaw, in part because contact rate is such an important factor. But it’s possible.

Protestors along 3rd Street allegedly set a police cruiser ablaze as thousands take to the streets near The Grove in Los Angeles. (Photo by Troy Masters)
And, in fact, it looks like that may be why the recent protests following the murder of George Floyd didn’t turn into engines of infection in most places. The protests amounted to a sudden, drastic – but very temporary – increase in the contact rate for those who participated.
But in many places the protests followed months in which strict isolation had driven prevalence down to very low levels.
They also occurred outdoors rather than indoors, and most participants wore masks, both of which would powerfully reduce infectivity. Under those circumstances, the reductions in both prevalence and infectivity may have balanced the sudden, very temporary surge in the contact rate, and we avoided major transmission events.
But unfortunately, that’s not what’s happening with the reopening in general.
Under our current leadership vacuum, we are deliberately engaging in a long-term increase in the contact rate while making virtually no attempt to tamp down prevalence or decrease infectivity to balance things out.
In the absence of a cure or an endless lockdown, prevalence is reduced when you test, contact trace and isolate infectious people. But while testing has increased, there are no nationwide or even statewide programs to isolate infectious people, which is the main benefit of testing. In some countries that have kept transmissions low, people who test positive are required to isolate at home.
Not urged to, required to.
They are constantly called and visited and otherwise monitored by public health workers, provided with food, medicine and other services, and repeatedly re-tested until they clear the virus.
Countries like China go even further.
People who test positive are sent to so-called ‘fever clinics’ and are required to stay there until they test negative, usually about two weeks. Some countries do a combination. If you live alone, they require you to isolate at home. If you live with others whom you might infect, they send you to isolation clinics.
Testing alone doesn’t do much unless you provide a safe, comfortable, humane and cost-free way to briefly isolate the infectious. But we’re not doing that.
As a result, we’re not addressing prevalence at all.
And when it comes to infectivity, reckless politicians are actually encouraging people to abandon masks, ignore social distancing, gather indoors, etc.
Under these circumstances, what’s happening with the reopening is this. We are increasing the contact rate significantly by reopening, but we’re doing nothing to tamp down prevalence and we’re actually increasing infectivity.
This is virtually a textbook definition of how you stoke an epidemic.
All this being true, I’m not particularly optimistic about the future even in places like New York, New Jersey and Connecticut that seem to be doing well at the moment. The tri-state region is almost certainly doing well because the lockdown and social distancing were extremely strict, which reduced prevalence to very low levels. But as the region reopens without a way to quickly identify pockets of infection and isolate the infectious, and without mandatory adherence to masks and other methods of reducing infectivity, transmission will eventually go back up. It’s just going to take a bit longer.
The good news is that epidemiologists know what we need to do to bring transmission under control. These principles have been well understood for over 100 years. And in places like Singapore, Hong Kong, South Korea, Vietnam, New Zealand, even China itself, where the virus has been largely eradicated, success has come by addressing all three factors of Prevalence, Infectivity and Contact Rate.
The results have been impressive. Life has returned to a semblance of normal and the inevitable minor outbreaks are quickly identified and stamped out.
The question is, do Americans have the ability – or the will – to do that here?
And do leaders even understand what we need to do?
For example, I keep hearing well-meaning politicians talking about the importance of testing, which is fine. But I almost never hear them go on to stress the importance of isolation, which is the main point of testing.
In the end, without a clear understanding of how epidemics work, we exist at their mercy.
And as humanity has learned repeatedly since time began, epidemics have no mercy at all.
— Gabriel Rotello is author of the 1997 book, “Sexual Ecology: AIDS and the destiny of gay men,” a book about the epidemiology of HIV and co-founder of OutWeek Magazine. He is currently a television writer, producer and director living in Los Angeles.
COMMENTARY
From rhetoric to persecution: When the State labels trans people as terrorists

In Los Angeles, where rainbow flags line Santa Monica Boulevard and queer communities carve out space to thrive, it can feel surreal that the federal government might one day classify transgender people as terrorists. Yet this no longer belies a paranoid fantasy. Reports surfaced this fall that the FBI is considering whether to categorize trans people under a newly minted threat label called “Nihilistic Violent Extremists”. This came in the wake of conspiracy theories that Charlie Kirk’s assassin was trans–theories that were later debunked. The Heritage Foundation, through its Project 2025 blueprint, has openly suggested that “transgender ideology” belongs in the same basket as terrorism. What sounds like fringe demagoguery is being whispered in the corridors of federal power.
The danger of such framing is terrifying. When governments confuse identity with ideology, they are laying the groundwork for persecution. We have seen this playbook before. In the 1930s, Adolf Hitler’s regime did not begin with concentration camps. It began with words. Jews were depicted as corrupting influences, dangerous parasites, and threats to Aryan purity. Bureaucratic edicts stripped them of jobs, banned them from public schools, and erased their presence from civic life. This sort of parallels what is happening to trans people right now–we have been banned from the military, we can’t use the bathroom of our choosing, and we are being denied critical healthcare. A rhetorical shift–from neighbor to danger–makes it possible for ordinary citizens to tolerate, and even participate in, their eventual destruction.
On his first day back in office, Trump signed Executive Order 14168, erasing gender identity from federal recognition, cutting funding for care, and redefining sex as fixed and immutable. Another order, 14190, criminalizes teachers who affirm a student’s pronouns or facilitate their social transition, equating simple recognition with exploitation. These are not abstract debates over language. They are policies that dictate whether people can live authentically, whether youth can find safety in schools, and whether families can see their children treated with dignity. To then float the idea of designating trans people as extremists is not an isolated thought experiment. It is a continuation of a campaign already intent on erasing us.
Just as Hitler began by classifying Jews as subversives, today’s political leaders risk classifying transgender people as national security threats. In both cases, identity is treated as a contagion. In both cases, the state deploys the language of danger to justify measures that would otherwise be unthinkable. And in both cases, the consequences for silence are catastrophic. When trans existence is conflated with terrorism, it becomes easier for ICE to surveil us, for policymakers to justify banning our gatherings, and for agencies to deny us access to the very structures of public life. What begins as words in a memo can end in barbed wire, if history is any guide.
Los Angeles knows better than to believe itself immune. The city has long been a sanctuary for queer and trans people, a place where art and activism have fused into survival. Yet federal classifications do not stop at county lines. A Pride march in West Hollywood could be branded a security risk if Washington decides that trans identity itself is extremist. A parent advocating for their child at a Los Angeles school board meeting could suddenly find their activism logged in a federal file.
The stakes of this moment are enormous. If the American public shrugs at the possibility of transgender people being labeled “nihilistic terrorists,” we risk normalizing the logic of persecution. And if that logic hardens, it will not stop with us. Once a regime learns to brand identity itself as dangerous, it will reach for new scapegoats to sustain its power.
Los Angeles has always been a city of resistance, a place where queer life refuses to be hidden, a place where silence is not an option. That spirit must animate our response now. To accept these federal whispers as mere rhetoric is to betray the lessons of history. To resist them is to defend not only transgender lives, but the integrity of democracy itself.
Words prepare the ground for action. Plenty of dictators have taught us that. The only question is whether we will recognize the warning signs in time.
Isaac Amend is a writer based in the D.C. area. He is a trans man and was featured in National Geographic’s “Gender Revolution” documentary. He serves on the board of the LGBT Democrats of Virginia and is a Yale graduate. You can follow him on Instagram at @isaacamend
Commentary
PrEPARING California for the future and better supporting those living with HIV
AB 554 is a huge step in the right direction; however, without consistent leadership from policymakers, those living with HIV will continue to be the first on the budget chopping block.
When I learned I was living with HIV nine years ago, there were a lot of questions to be answered: how will I access treatment? Will I feel safe and respected by my care team? What does stigma look like for me in the fourth decade of the HIV epidemic?
While I was fortunate to have a wonderful team of case managers and health care providers who guided me through an unfamiliar and complex medical system, I’ve heard countless stories of people fighting tooth and nail just to find appropriate care, let alone treatment.
Our country’s labyrinthine, convoluted health system is cluttered with obstacles like prior authorization and step therapy. Both of which needlessly delay access to health care by imposing vague requirements and/or forcing patients to “fail” a series of medications before they are granted access to the one actually prescribed by their physician. For game-changing HIV prevention drugs like PrEP, these hurdles endanger lives. Combined with our current federal landscape being incredibly antagonistic (i.e., the Trump Administration trying to gut $1.5 billion in HIV prevention funding, among a laundry list of offenses), the LGBTQ+ community is facing disproportionate hardships that are exacerbating disparities and contributing to further stigmatization.
Thankfully, California policymakers are doing their part to protect our community. Assembly Bill 554, authored by Assemblymember Mark González (D-Los Angeles), follows in the footsteps of nine other states by ensuring coverage for all long-acting, injectable drugs used for PrEP and PEP. The bill “safeguards patient and provider choice” by eliminating cost-sharing and expanding access to a wider range of ARV medications to help bolster medication adherence rates. It also ensures coverage for future formulations of ARV drugs that are better at making HIV undetectable and untransmissible.
PrEP (pre-exposure prophylaxis) and PEP (post-exposure prophylaxis) are effective regimens for preventing the transmission of HIV when taken as prescribed. AB 554 enshrines quick access to these treatments, satisfying calls for health equity, especially for Black and Latino Californians, who face disproportionate transmission and infection rates.
AB 554 is a huge step in the right direction; however, without consistent leadership from policymakers, those living with HIV will continue to be the first on the budget chopping block. Just last week, the California Legislature passed a budget trailer bill (AB 144) that includes provisions to divert funds from the AIDS Drugs Assistance Program Rebate Fund toward general state operations.
California policymakers can’t say they’re countering the Trump Administration and supporting the HIV community if they’re also ripping the rug out from underneath us. AIDS Drug Assistance Programs are lifelines – they normalize diagnoses, fund direct services, and help uninsured and underinsured patients access essential care.
Ironically, while AB 554 will build upon the work of ADAPs to eliminate prohibitive barriers, AB 144 will steal funds from the program to instead boost state revenue. ADAPs already operate from a very small annual revenue of fixed federal funding awards per state. States taking more money away from these critical programs will threaten their ability to serve HIV patients. Moreover, these dollars are statutorily prohibited from being used for non-HIV care by Title II of the Ryan White CARE Act.
California is destined to repeat the sins of the past unless Governor Newsom steps in. For too long, those living with HIV have been isolated, cast aside, leveraged for political gain, and dropped soon thereafter if something better comes along. We are not budget dust, we are not pawns in a political game, we are real people with real voices, and we’re asking Governor Newsom to do what’s right: redline the ADAP provisions from AB 144 and sign AB 554 into law.
California can lead the nation in doing what’s right for all communities. But it starts with policy, and we have to make sure policies are centered around those they impact.
Kalvin Pugh is the state policy director for the Community Access National Network, a national 501(c)(3) nonprofit that works to improve access to health care services and supports for people living with HIV/AIDS and viral hepatitis through advocacy, education and networking.
Commentary
Pride & promiscuity: What the current face of gay sex culture says about us
A dive into the historical, social, and psychological motivation that drives us into each other’s arms.

As gay men, are we having more sex than our fore-daddies or just more open about it? Between Grindr dings that hit harder than Double Scorpio, PrEP prescriptions as our daily gay-ly vitamin, and the ever-present anxiety of FOMO, I think it’s fair to ask, is hooking up becoming a numbers game, more focused on quantity vs. quality, for many of us ‘mos?
For eons, gay sex has been both a subject of fascination and moral panic for those on the hetero side of the picket fence. But the conversation has shifted. Today, the questions come less from pearl-clutching conservatives and more from within our own community. How much is too much? Are we liberated yet? Are more and more of our gay brethren basking in the waters of heteronormativity? And to what extent are our sex lives driven by libido, validation, or the simple fact that we can?
Let’s start with the obvious culprit: technology. Of course, as gay men, the first thing that we did following the birth of the smartphone was create a way to see all of the fair-game dick within a one-mile radius. We were the first to adopt hookup apps as essential social tools, from the early days of Grindr to the onset of Sniffies. According to research cited by Gay Counsellor, compulsive use of apps can mirror patterns of behavioral addiction, where “likes” and “messages” stimulate dopamine in ways eerily similar to gambling. The buzz of a notification becomes less about actual intimacy and more about self-worth. Sex as currency, matches as validation.
A TIME article warned in 2014 that hookup apps might be “destroying gay relationships,” arguing that the sheer efficiency of digital cruising left little incentive for building intimacy. Why invest in a partner when you can have instant access to some NSA ass five feet away? It’s the Amazon Prime of getting off – quick delivery, same-day service.
I think that these critics are missing a nuance here. Apps aren’t inherently bad; they are simply adding a Cialis to what’s already in our culture. If we already treat sex as a form of transactional validation in normal life, apps inject that insecurity with steroids.
Then there’s PrEP, the little blue pill that revolutionized sexual health and, in turn, our sex lives. Since its FDA approval in 2012, Truvada has been both a miracle and a lightning rod. A CUNY study found that PrEP has fueled perceptions of promiscuity. The assumption is that biomedical safety nets invite reckless raw-dogging abandon, reinforcing the stereotype of gay men as hedonistic ho-bags.
But the data tells a more complicated story. Research published in the Journal of Medical Internet Research (2022) suggests that while PrEP use does correlate with higher numbers of sexual partners for some, it also fosters healthier discussions about safety and reduces anxiety around HIV. Translation: PrEP doesn’t make people slutty, it makes them feel secure. If this sense of sexual security emboldens them to embrace their sexuality more fully, is that really a problem? Or is it just a shift in norms?
Of course, none of this exists in a vacuum. As The Conversation notes, homosexuality may have evolved as much for social bonding as it did for reproduction. Historically, gay sex wasn’t just about pleasure but also survival, solidarity, and even networking. In the years after Stonewall, sex was political. It was a sweaty form of protest against heteronormative repression, a celebration of community in defiance of shame.
But in 2025, sex has also become… a competition. Liam Heitmann-Ryce-LeMercier’s essay on Medium critiques how queer culture sometimes conflates liberation with obligation. Promiscuity is framed less as personal choice and more as proof of authenticity. Don’t want to sleep around? Then maybe you’re repressed, prudish, or not “gay enough.” The pressure cuts both ways – to have sex, to crave sex, to keep up with everyone else’s sex.
And here’s where FOMO comes in. For every wild Saturday night Instagram story, there’s someone scrolling at home, wondering if they’re missing out – not on an orgasm, but on acceptance and belonging. The sex itself is just the trophy to the win, secondary to the validation of being chosen, the real prize.
So what actually drives this culture? Libido is undoubtedly up in this. Gay men, like all people, are wired with sexual impulses. But the psychological factors are harder to ignore. Validation looms large. The “yes” of a stranger affirms desirability. The “no” can often feel like a reflection of our worth. Ego magnifies the stakes, turning sex from a dance in the sheets into a scoreboard.
A telling study in the International Journal of Environmental Research and Public Health posited that compulsive app users often report using sex as a coping mechanism for loneliness and low self-esteem. Which inevitably raises the question – are we having more sex because we want it, or because we need to prove something, whether that is to ourselves and to others?
No discussion of queer sex culture or sex as a whole would be complete without tackling entitlement. Many of us know the type: the man who can’t take “no” for an answer, who interprets rejection as an insult, who cloaks his bruised ego in accusations of rudeness or exclusion.
Here’s the truth: just because you hand out a cookie or two doesn’t mean you have to share with the class. Consent is not a punch card system, and no one is entitled to anyone else’s body. Yet too often, rejection is reframed as cruelty, with aggressors painting themselves as victims. Is it gaslighting? Maybe. Is it delusion? Almost certainly. The lesson is simple: declining sex doesn’t make you a monster, and other people’s inability to handle rejection doesn’t make it your problem. Autonomy is not negotiable.
So are gay men more promiscuous today? In some ways, yes. Apps have streamlined access, PrEP and doxy have lowered risks, and cultural stigma is withering. But promiscuity isn’t the villain or the hero of this story. It’s a spectrum, shaped by psychology, politics, history, technology, and so much more.
For some, sex is liberation; for others, it’s compulsion. For some, it’s community; for others, it’s ego. The pearl-jammed peril lies not in the sex itself but in mistaking quantity for quality, validation for value, or pressure for choice.
Our challenge isn’t to moralize but to contextualize. To ask ourselves (and only ourselves) not how much sex we’re having, but why, and to respect that everyone’s reasons for getting down are their own. And to remember that liberation isn’t measured by tallies on a jockstrap waistband but by freedom from stigma, coercion, and shame. Stay safe and stay self-aware, my fellow bedfellows.
COMMENTARY
From rhetoric to renewal: How we heal America together
We must reckon with the fire we’ve built around politics

Charlie Kirk was no stranger to controversy. He thrived in it. He built his career on standing at the microphone in crowded lecture halls and telling skeptical young progressives to “prove me wrong.” At just 18, he saw a vacuum on the political map and filled it, co-founding Turning Point USA, which now calls itself the largest conservative student movement in the nation. His reach stretched from high school classrooms to the White House, his podcast drawing millions, his organization boasting thousands of programs, and his presence sparking protests wherever he spoke.
Kirk’s sudden and tragic death has left America reeling. For his followers, he was a bold voice who gave them language to express frustration with the left. For his critics, he was a provocateur who stoked division for profit. But for all of us, his passing should force us to reckon with the fire we’ve built around politics. Because let’s be honest: it isn’t just rhetoric anymore. Words are hardening into violence. Ideas are becoming weapons. And a democracy that devours itself from within cannot endure.
America is fractured. Our civic life feels like it’s splintering beneath our feet. Whether you are gay or straight, trans or cisgender, conservative or progressive, the same truth echoes: hate is taking lives. Too often, leaders build their platforms not by lifting people up but by tearing communities down.
We’ve seen how quickly careless words can spiral into fear, how easily fear becomes cruelty, and how cruelty ends in tragedy. This isn’t about one man’s career or ideology. This is about us — a country that keeps choosing division over dignity, suspicion over solidarity. That choice is killing us.
In this moment, America needs courage. And often, that courage comes most clearly from the communities that have borne the brunt of hate the longest. LGBTQ Americans know what it means to be targeted, to be legislated against, to have their very existence debated in the public square.
And yet, despite that, queer communities have built joy. They’ve built love. They’ve built families, art, churches, businesses, neighborhoods — not in spite of being different, but because difference can be beautiful. That resilience holds a mirror up to America: this is what it looks like to endure, to rise above rhetoric, to keep creating hope even when the world insists you don’t belong.
It’s not the LGBTQ community that needs to be convinced of America’s worth. It is America that needs to be reminded of its own soul.
Dr. Martin Luther King Jr. spoke of a dream where children of every race could sit side by side in dignity. Today, that dream must stretch wider. It must include queer children who deserve safety, trans youth who deserve freedom, and every marginalized person who deserves to breathe the air of equality without fear.
But make no mistake: this dream will not be realized by vilifying those with whom we disagree. It will not be achieved by mocking faith or silencing the voices of the right. It will come only when conservatives and progressives, red states and blue, stand together and admit that diversity is not America’s weakness — it is America’s genius.
To those on the far right who fear LGBTQ neighbors: your fear is misplaced. The call is not to give up your faith or your freedom. It is to recognize others’ right to theirs. And when we recognize each other’s humanity, the promise of America is finally fulfilled.
What we must do now is clear. If America is to survive this age of division, we must begin by reclaiming empathy. That means looking beyond the noise of politics and policy to truly see one another as human beings — neighbors, families, and communities whose dignity is not up for debate. We must protect the vulnerable, standing firmly with LGBTQ youth, immigrants, people of color, and all who have been pushed to the margins of society. Their safety and belonging cannot be treated as optional. We must celebrate difference, treating diversity not as a problem to be managed but as one of our nation’s greatest gifts. Our strength has always come from the kaleidoscope of identities, cultures, and voices that call this country home. And finally, we must hold speech accountable. Words shape worlds. When leaders choose language that harms, divides, or stokes fear, they corrode democracy itself. When they choose words that heal and summon courage, they open the door to renewal. Only when we embrace these commitments can we move from rhetoric to renewal—and begin the work of healing America together.
Charlie Kirk’s life was proof that words carry weight. His death must remind us that the weight of our words can no longer crush the spirit of this country. The question before us is not whether America will be divided — it already is. The question is whether we will summon the courage to heal it.
The time for slogans and soundbites has passed. The time for renewal is now.
Because if America continues to treat difference as danger, then democracy itself will wither. But if we choose to see difference as destiny, then we can build a nation strong enough to hold us all. That choice is not theirs. It is not mine. It belongs to all of us. And history will remember what we decide. Only when we embrace these commitments can we move from rhetoric to renewal—and begin the work of healing America together.
Emma Roshioru is a senior at Virginia Tech majoring in Political Science and Public Relations. Dr. James Bridgeforth is an independent, nationally syndicated columnist whose work has appeared in the Los Angeles Blade, The Washington Post, and the Washington Examiner.
Commentary
Don’t miss the liberation in the silencing of Charlie Kirk
In the aftermath of the assassination, we are now drowning in a pool of speech violence that could lead to an American catastrophe.

Trans advocates have argued for years that anti-trans speech leads directly to anti-trans violence, and were eye-rolled to oblivion. Charlie Kirk, whether as a mouthpiece for what politicians dared not say out loud, or as a hype man keeping the politics of resentment ever inflamed, built a career out of weaponizing right-wing talking points, fueling a culture of violence that ultimately killed him, and now threatens all of us.
The trail of harm caused by Kirk’s rhetoric is not abstract—it lines up with real blood and real deaths. When he blasted the phrase “China virus” into cultural discourse—parroted days later by Trump—anti-Asian hate crimes spiked. His COVID misinformation spread right alongside hundreds of thousands of needless fatalities. When he compared abortion to the Holocaust, he sanctified the moral panic that cleared the way for Roe v. Wade’s destruction—and pregnant people now die totally preventable deaths like it’s 1972 again.
Kirk also called gender-affirming care for youth “child mutilation,” language now enshrined in legislation that has severed a lifeline for vulnerable kids and their families. He urged that trans people be “taken care of the way society handled us in the 1950s and 60s,” that is, with lobotomies, shock therapy, and police persecution. He spent his last moments on earth promoting the conspiracy theory that trans people make up an imaginary majority of mass shooters—classic fascist scapegoating with the obvious aim of inciting more violence against trans people.
The irony cannot be overstated that his actual last words, spoken as he was shot, minimized the human toll of gun violence. In death, Charlie Kirk proved the point that sowing violence with words reaps real-world tragedy. He gave trans activists the last word on the matter forever.
And now we know the truth: Kirk was not killed by a leftist or a trans activist, but by Tyler Robinson—a young white man evidently radicalized by the toxic masculine internet culture that Kirk and his allies normalized. When you cultivate a culture of hate and fear, when you normalize conspiracy and scapegoating, when you insist that violence is the only solution, eventually your own people will turn those weapons back on you. And your personal world is left bereft and traumatized, just like the 47,000 families affected by gun violence last year alone.
In the aftermath of the assassination, we are now drowning in a pool of speech violence that could lead to an American catastrophe. That is, it does if we miss the opportunity for real liberation that it offers us.
The Right cannot stop itself from using speech violence—terror carried out with words, designed to destabilize and intimidate. In the hours after the assassination, Republican leaders used Kirk’s blood to paint a target on our backs, issuing statements rife with misinformation that unleashed a wave of bomb threats across the country, forcing schools, hospitals, and community centers to evacuate.
It seems as if they know no other language. But do we? Or have we become radicalized in the same way, just with different targets? Understandable as it may be, and satisfying as it may feel, the Left’s memefied celebration of Kirk’s death only amplifies the violence he put into the world.
A friend told me about a teacher at their children’s Miami school who tweeted “Karma’s a bitch;” the school was immediately bombarded with mass shooting and bomb threats. I am publishing this article anonymously due to the doxxing and threats happening to anyone who doesn’t lionize Kirk online right now. I won’t be silenced, but I won’t risk my own physical safety, either, and that is how bad it really is right now. This even causes me to question my anger at Center-Left figures like Gavin Newsom, who seem to be glossing over the harm Kirk caused in his life in their public statements—maybe they’re just afraid of getting assassinated themselves.
We have to see the bigger picture: only Right-wing politicians and billionaire-owned platforms profit from making Americans hate each other to the point of physical violence. Speech that incites violence is not freedom of expression; it is a tool of fascism. It sows chaos, breeds fear, normalizes inaction, allows politicians to consolidate power, and enables the ultra-wealthy to “buy the dip,” profiting off instability. At the end of this cycle, ordinary people will be less safe, less free, and more hopeless—unless we end it.
One of the most radical progressive things we can do right now is refuse hate speech altogether. We have an opportunity to liberate ourselves by creating where Kirk sought to destroy. Stop participating in this angry tit-for-tat, regardless of how righteous your emotions may feel. Don’t share the memes. Don’t feed the cycle. Don’t let your kindness and goodwill corrode by mimicking the hate Kirk aimed at us.
Roll your eyes, but also consider this approach: When you feel the urge to fire back online, step away. Then imagine a possibility. Then take one action that feeds your soul. Call a friend. Organize something that makes your community measurably better. God knows, the Left needs a plan right now—we can use these provocations as fuel to build one.
Of course, it takes a kind of saintly strength to live this principle—one I’m not sure any of us possess right now. But we can resist fascism if we start by noticing the urge to answer hate with hate, and jiu-jitsu that energy into strengthening ourselves and our communities.
Remember the classy response to the death of Fred Phelps, leader of the hate organization also known as Westboro Baptist Church. Queer activists held signs for his family to see at his funeral: WE ARE SORRY FOR YOUR LOSS. Members of his family have since become outspoken against their own work. A few picketers still find their only meaning in protesting funerals, but when was the last time you ever cared about that sad little man, or what he did?
One head of the Far Right media ecosystem hydra has been cut off. That is not a cause for celebration, but it is a real opportunity. Figures like Charlie Kirk are not just another talking head—he was a cult figure who can’t simply be swapped out. There is now a vacuum, and the questions remain: Who fills it? With what?
We have just inherited the gift of a world free of Charlie Kirk’s vitriol. Instead of polluting our future with more of the same, let’s seize this opening and direct our energy toward manifesting the world we wish out loud for every day.
A popular 1980s slogan in the LGBTQ+ community was “We are everywhere.” We truly are part of every profession, every race, gender, class, religion, and more.
Just as other communities have media outlets that take a “by us, for us” approach to news and information, there has been a gay press in fits and starts going all the way back to 1924, when a U.S. postal worker named Henry Gerber and his pals launched Friendship & Freedom in Chicago. The police arrested Gerber and shut the newsletter down.
More than 100 years later, the state of LGBTQ+ media might be better than what Gerber experienced, but due to discrimination and political headwinds — including corporate backsliding on diversity marketing — there is a struggle to serve the community with strong local LGBTQ+ journalism.
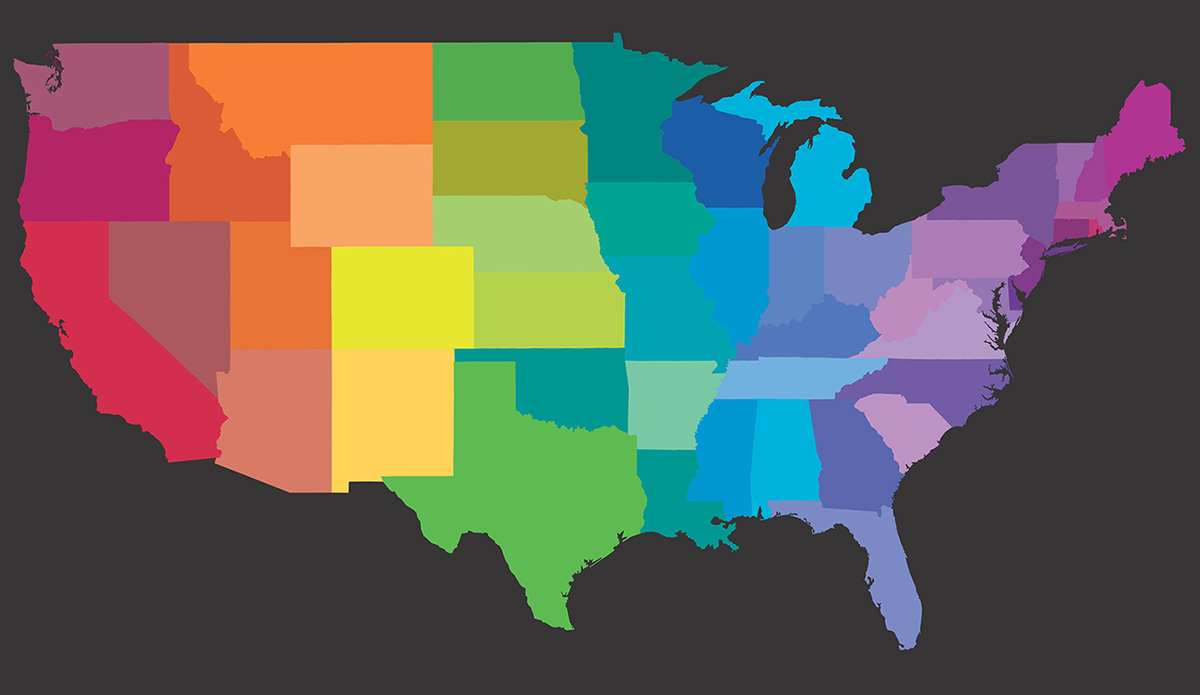
Which is why I set out in late 2024 to start to document the current state of local LGBTQ+ media in the U.S. Thanks to a grant from the MacArthur Foundation, The LGBTQ+ Media Mapping Project, hubbed at the News is Out collaborative sponsored by the Local Media Foundation, is now available. With a map developed by City University of New York’s Craig Newmark Graduate School of Journalism Center for Community Media, we have a better sense of the strengths and weaknesses facing this niche within the media world.
While I had published a book on LGBTQ+ media several years ago (Gay Press, Gay Power), I still was not prepared for just how precarious this media ecosystem is today. Our report found 18 states with no LGBTQ+ media and that many city-based media are unable to cover their entire states. Millions of people have no local LGBTQ+ media coverage.
During focus groups, we asked the publishers and editors just what needs they have, beyond an obvious infusion of cash. They are seeking to diversify their revenues, to adapt to new technologies, grow their audiences, and to better serve neighboring communities. There are a wide range of recommendations in the report, things the outlets themselves see could be valuable.
Philanthropy has barely stepped into this part of the media universe in part because almost all LGBTQ+ media, both local and national outlets surveyed, are for-profit. But now that more funders see a need to support local for-profit media, this could open up an opportunity to support more of these outlets. Given the political backlash against the community, now is not the time to push these businesses to become non-profit, as that could be a new single-point failure.
Our report also found that during this time of crisis, there has been a surge in audience, and more willingness to work together. The participants in this research indicated a strong willingness to collaborate across both business and editorial opportunities. But such efforts require an investment of both time and money. Support is needed.
We surveyed both legendary local LGBTQ+ newspapers and newer online outlets. More research should be done on the creator/influencer world, which includes many LGBTQ+ people. And while local LGBTQ+ media was the primary focus of this research, we did survey national LGBTQ+ media. I was surprised how precarious many of these outlets are as well.
The entire LGBTQ+ media universe could use a strategic plan and an infusion of new resources, which I hope funders will step up to support.
In the meantime, readers can support LGBTQ+ media by signing up for their newsletters, and donating or subscribing if they have those options.
Please see the report for a full slate of recommendations, here: https://newsisout.com/lgbtq-media-mapping/. The map is hosted on the Craig Newmark Graduate School of Journalism website here: https://lgbtqmediamap.journalism.cuny.edu/ . We will update the map as new outlets are found; indeed, we have already added new dots to the map.
Tracy Baim is the co-author of The LGBTQ+ Media Mapping Project report with Hanna Siemaszko. She is the co-founder of the 40-year-old Windy City Times LGBTQ+ newspaper, and is the executive director of Press Forward Chicago, a journalism pooled fund part of the national Press Forward movement.
Commentary
Claiming space, leading boldly: A new chapter in HIV fight
A time of extraordinary possibility and profound peril

I step into the leadership of the National Minority AIDS Council at a time of both extraordinary possibility and profound peril. We are living in a moment where science has given us the tools to end HIV as a public health threat—PrEP, PEP, U=U, long-acting injectables, and decades of research that have transformed what was once a death sentence into a manageable condition. And yet, the systems meant to deliver these tools are under siege.
Public health is being politicized. Science is being undermined. Civil and human rights are being rolled back. The safety and security of LGBTQ+ people—especially Black and Brown queer and trans folks—are increasingly fragile. In some states, even saying the word “gay” in a classroom is considered controversial. In others, access to gender-affirming care is being stripped away. And all the while, HIV continues to disproportionately impact communities that have been historically marginalized and medically neglected.
So yes, I step into this role with a sense of urgency. But I also step in with pride. Because I know what it means to be underestimated. I know what it means to be told you don’t belong. As a Black, church-going, gay boy from the South Side of Chicago, I grew up in a world that didn’t always see me, didn’t always protect me, and certainly didn’t expect me to lead a national movement. But here I am. And I’m not alone.
I carry with me the legacy of those who came before—of Marsha P. Johnson and Bayard Rustin, of Magic Johnson and Ryan White, of the activists who lay down in the streets and shouted “Silence = Death” until the world finally listened. I carry the wisdom of Black grandmothers who raised generations through grief and grit. I carry the fire of young people who refuse to be silent, who organize, who vote, who demand better.
At NMAC, we are not just fighting a virus, we are fighting the systems that allow it to thrive. We are fighting racism in healthcare, transphobia in policy, and stigma in every corner of society. We are fighting for Black and Brown communities, for LGBTQ+ youth, for aging people living with HIV who deserve dignity, not invisibility.
This is not just a job, it’s a calling. And it’s a call to action for all of us.
We must raise our voices louder than the attacks. We must claim space in rooms that were never built for us. We must demand funding that reflects the urgency of our communities’ needs. We must protect the programs that work—like Ryan White, HOPWA, and PEPFAR—and expand access to innovations like long-acting PrEP.
We must also tell the truth: that ending the HIV epidemic is not just a scientific challenge, it’s a justice challenge. It requires confronting poverty, housing insecurity, criminalization, and the erosion of civil rights. It requires centering people who live at the intersection of multiple oppressions. It requires love, radical empathy, and unapologetic leadership.
I am ready to lead. But I cannot do it alone.
To every activist, provider, policymaker, and person living with HIV: this is your movement too. Your voice matters. Your story matters. Your survival is revolutionary.
Let’s build a future where HIV is no longer a threat—not because we ignored it, but because we faced it head-on. Let’s build a future where public health is protected, science is respected, and every person—regardless of race, gender, or sexuality—can live with dignity and thrive.
Let’s build it together.
Harold Phillips is incoming CEO of National Minority AIDS Council.
COMMENTARY
A call to act, not just observe, this Suicide Prevention Month: If we meant it, we would fund it
Despite September being Suicide Prevention Month, crucial mental health are being defunded across the country. Real prevention needs more than awareness campaigns.

September is Suicide Prevention Month, a time to address often-ignored painful truths and readdress what proactivity looks like. For those of us who have lost someone they love to suicide, prevention is not just another campaign. It is a constant pang that stays.
To lose someone you love to suicide is to have the color in your life dimmed. It is beyond language. Nothing one can type, nothing one can say to a therapist, no words can ever convey this new brand of hurting we never imagined before. It is an open cut so deep that it never truly, fully heals.
Nothing in this world is comparable to witnessing someone you love making the decision to end their life because they would rather not be than to be here. Whether “here” means here in this time, here in this place, or here in a life that has come to feel utterly devoid of other options, of hope, or of help, the decision to leave often comes from a place of staggering pain and a resounding need to be heard. The sense of having no autonomy, of being trapped inside pressure so immense it compresses the will to live, is no rarity. It is a very real struggle that so many adolescents and young adults carry the weight of every day.
Many folks in our country claim to uphold the sanctity of human life. But if that claim holds any validity or moral grounding, it would have to start with protecting the lives of our youth. Not only preventing their deaths but affirming and improving the quality of their lives. We need to recognize and respond to the reality that for too many adolescents and teenagers, especially those who are marginalized and chronically underserved, life does not feel so sacred. It feels damn near impossible.
Today, suicide is the second leading cause of death for Americans ages 10 to 24. That rate has almost doubled since 2007. Among queer-identifying youth, the statistics are crushing. Nearly 42% have seriously considered suicide in the past year, and almost 1 in 4 have attempted it. These are not just numbers. These are the children and teens we claim to care for and protect. These are kids full of potential and possibility who come to believe that their lives are too painful or meaningless to go on.
For our youth who identify as both queer and BIPOC, the numbers soar to even more devastating heights. Discrimination, housing insecurity, trauma (complex, generational, or otherwise), and isolation pile on the already stacked mental health risks. Transitional times like puberty, continuing education, coming out, or even being outed can all become crisis points. And yet, the resources available to support these youth remain far too limited, particularly in rural and underfunded communities.
We must also call out a disheartening truth. Suicide is not just a mental health issue but also a political one. Despite years of advocacy and an undeniable increase in youth mental health crises, funding for prevention is barely pocket change in regard to national budgets. In 2023, the federal government spent an underwhelming $617 million on suicide prevention efforts. To provide some perspective, that’s less than what we spend each year defending the border wall.
Meanwhile, school-based mental health services, one of the most effective means of reaching children and teens early, are being decimated. A $1 billion mental health grant program, which began after the Uvalde school shooting aiming to increase school counseling services, was recently pulled from hundreds of school districts. In some places, that left over 1,000 students for every 1 mental health provider. And in others, it left entire counties with zero youth therapists.
This rollback is not an isolated agenda. It operates in tandem with a cultural and legislative attack on the LGBTQ+ community and our access to affirming education, healthcare, and visibility. Programs that create safe spaces and lifelines are being wiped away. The LGBTQ+ line of the 988 suicide hotline, created to offer identity-affirming, culturally competent crisis support, was recently defunded, despite having provided help to over 1.3 million callers. The political message here is unmistakable. Only some lives, some pain, and some needs of a select group are worth the money and care.
I can’t help but contrast this with how our country controls the process of childbirth. Over the last decade, particularly following growing awareness and resulting concern around maternal mortality rates, the U.S. has consistently increased investment in maternal health. Federal funds now support initiatives like Healthy Start, safety improvements in birthing facilities, and dedicated maternal mental health hotlines. In 2022, the Into the Light Act was passed, allocating $170 million over six years for screening and treatment of postpartum mental health conditions. These are great and necessary efforts. But even here, we fall short. A study published in JAMA Psychiatry in November 2023 examined drug overdose deaths among pregnant and postpartum women in the U.S. from 2018 to 2021. The findings revealed that suicide and overdose were the leading causes of death during this period.
Yet even this limited progress for new parents shows us an undeniable contradiction. As a nation, we have shown we are capable of legislating support for life when we are politically and morally motivated to. We can pass bills, allocate funds, and create crisis hotlines. What’s missing is the motivation to extend that same urgency to the mental health and well-being of young people before they become statistics.
At the same time, astonishing amounts of public money have been directed toward restricting reproductive freedom. Since the overturning of Roe v. Wade in 2022, states have collectively spent hundreds of millions of dollars enforcing abortion bans, funding legal battles, surveillance infrastructure, and crisis pregnancy centers that often provide misleading information.
In 2023 alone, Texas allocated over $140 million to the Alternatives to Abortion program, while at the same time slashing funding to health providers that offered comprehensive reproductive care. Nationwide, anti-abortion lobbying and litigation have received sustained state and federal backing, often at the expense of preventive care, contraception access, and the very maternal health supports that claim to be prioritized. Only the willful can ignore the blatant contradiction here. While suicide and overdose silently claim the lives of mothers post-childbirth, far more political and financial energy is funneled into controlling whether people can become mothers in the first place.
Real prevention should not be limited to easy words and good intentions each September. Real prevention should be about intrenching mental health support into the daily lives of young folks. It means funding school counselors and social workers so that every child has someone to talk to. It means restoring services that center the needs of queer, Indigenous, and BIPOC youth, who are far too frequently left behind. It means guaranteeing that crisis lines are open. It means creating and nurturing environments where vulnerability is not discouraged but invited.
We also have to stop criminalizing mental health crises. Way too often, suicidal and struggling youth are met with handcuffs or hospitalization that adds layers to trauma rather than with compassion. Prevention must be proactive, not punitive. We need peer support groups, trauma-informed teachers, and trusted adults who are trained to notice the signs before the worst happens.
We are also overdue for a culture shift. A society with the alleged aim to value life does not shame those who are struggling to hold onto it. Contrary to popular unsaid belief, strength is not stoicism. Strength is connection. It’s knowing when to ask for help.
If we as a country actually and honestly cherish life, we have to prove it. We have to prove it not with words but with resources, policy, and compassion. Suicide prevention cannot begin and end with simple slogans and annual awareness. It has to mean a continuous investment in systems of care that affirm life, especially for those who are most vulnerable.
This September, as we recognize Suicide Prevention Month, I dare us to do more than to just memorialize those lost. Let’s start fighting for those living. Let’s create a world where no child, teen, or young adult feels that their only way out is to stop living. They are not expendable. They are not alone. And their lives are sacred. If only we had the heart to act like it.
I am almost ashamed to say that it wasn’t until I lost someone I love to suicide that I began volunteering my time to the American Foundation for Suicide Prevention. The work that the AFSP does is not only needed, it’s imperative today more than ever. If nothing else, please hit this link and donate.
Commentary
Lil Nas X and the cost of being seen
We praised his defiance and ate up his content, but now that he’s hurting, how can we show up? What Lil Nas X’s recent struggle says about us.
At a time when the world feels like it’s already choking on mouthfuls of disheartening news every day – genocide on the Gaza strip, climate crisis, political descent here and abroad – the last thing any of us want to hear about is another headline on a young star reportedly hospitalized following a possible overdose. Yet here we all are, watching a very familiar pattern unfold. This time, it’s our beloved queerby Lil Nas X.
According to TMZ, Lil Nas X, né Montero Lamar Hill, was reportedly hospitalized for a possible overdose mere months after he opened up publicly about how difficult the last few years of his career have been. He took to social media, stating, “I jumped straight into adulthood with extreme fame around me. So it was really nice to be just outside walking and meeting people in the streets and eating at restaurants, just even alone, spending a lot of alone time in solitude.”
Sound familiar? It should. The razzle-dazzling surface of fame seldom shows us the internal clutter and chaos, the pressure, the expectation to always be on, meanwhile mental health is brushed aside. And for our queer artists, particularly Black queer artists like Lil Nas X, the burden becomes that much denser.
We’ve seen this before. Demi Lovato. Aaron Carter. Whitney Houston. Talented, beloved artists who, for one reason or another, found themselves unraveling under the unrelenting scrutiny and chaos that comes hand in hand with fame. Some of them make it through. Some don’t. Many cry for help ages before things reach a breaking point. But what did we do? Did we listen? Did we leave Britney alone? Or are we the ones who light the match, pull out our phones, and film the flames? For once, please don’t tag me.
Lil Nas X sashayed onto the scene not just as a chart-topping artist, but as a cultural disruptor. Diva wore dresses to award shows. He clapped his cheeks on Lucifer in the music video for Montero. He vogued his way into the conversation on gender, sexuality, religion, and race that made a whole lot of folks uncomfortable, and that was the point. We were living for it, for him. We liked, we shared, and we reposted. We ate it tf up and licked our fingers clean. But did we ever truly care?
When a person like Lil Nas X steps out of the spotlight to say, “I’ve been having a hard time,” do we respond with any empathy, or just wait around for the next head turning lewk or satanic lapdance? It’s easy to forget that behind the headlines is a real human. One with a nervous system, a childhood, a family, and so much more. And, what most often goes ignored by all, a limit.
There is something particularly painful about seeing this happen to queer people in the public eye. We’re told that visibility is freedom. And to an extent, it is. Lil Nas X became a rare symbol of queer Black excellence in mainstream media, an unapologetic icon. But visibility without protection has the potential to be fatal. Fame doesn’t guarantee safety – not physically nor emotionally. As a matter of opinion, for queer people, it’s more often than not the opposite.
When you’re queer in the spotlight, you’re performing resilience first and music second. You’re expected to rise above, to remain unbothered, to smile at all times no matter the weight of the pressure, to be a walking teachable moment at every moment. And when you break down? People either turn their backs or turn you into a meme.
FACT: mental health in the queer community is already a crisis. Study upon study have consistently shown that LGBTQ+ identifying folks are at significantly higher risk for anxiety, depression, and suicide. Add international stardom to the mix, and you don’t get immunity from this. You get fast-tracked.
And yet, we continue to lap up these public struggles like entertainment. The media machine feeds on our thirst, and we keep clicking. Headlines about a “possible overdose” become the most clicked clickbait. Tweets become jokes. Vulnerability becomes viral.
So then we have the question, what does it mean to authentically support an artist like Lil Nas X, not just when he’s on stage, but when off stage as well? When the posts stop posting. When the glitter dulls. Are we prepared to support our icons through their harder times the way we do when they’re on top of the world?
We can start by changing how we engage. Honestly take a moment to ask yourself, are you clicking on these stories to gag or to understand? Are you giving compassion or commentary? Are you holding a mic to their cry for help, or are you fetishizing their struggle?
We also need to shine a light on the entertainment industry to offer real mental health resources and protections, especially for young and marginalized artists whose career they are both responsible for and profit immensely from. Care does not come hand in hand with fame. It’s often the reason care is a concern.
We don’t know the full story of what happened with Lil Nas X, and jumping to conclusions is like eating at Chick-fil-A: only those of low intellect are tempted. But what we do know is that someone allegedly ended up in the hospital after publicly saying they were struggling. That alone should be enough to warrant concern. Not for the gossip or clicks but for simple humanity.
Commentary
Over the Rainbow: The systemic rollback on LGBTQ+ Rights
From erasing rainbow crosswalks to defunded healthcare, queer communities are sitting front row to a coordinated effort to strip away decades of progress. Take this as a call to pay attention, and to action, before more rights quietly vanish.

In the past decade, rainbow-clad crosswalks have popped up in cities across our country, serving as affirmations of long-overdue queer solidarity and resilience. But today, in more and more places, those colors are now being scrubbed away, painted over, and banned under new regulations. What may seem to some as an inconsequential repaving is, in reality, a call to action. It signals a shift away from inclusion, toward an erasure and the sanitizing of public spaces where visibility is becoming, once again, a luxury for select populations. This is not a simple matter of public art. It’s a matter involving power, belonging, and the right to exist as who we are.
Let’s see this for what it is. In stripping away our technicolor stripes, we also lose the unspoken sense of safety and acceptance that they provide to so many who need just that. Rainbows speak to an array of identities and experiences. Taking this away signals a return to conformity, and ultimately, invisibility. These crosswalks have long functioned as not just decoration but straight-up declarations. They say to LGBTQ+ pedestrians “You belong and you belong here.” Taking away these symbols actively communicates something just as loud yet far more bleak… “Not anymore.”
The erasure of Pride-themed crosswalks echoes a consistent pattern seen throughout American history where public symbols tied to marginalized groups are challenged, removed, or reframed under the gaslighting of neutrality and “tradition.” Just in the past few years, murals honoring Black leaders or giving voice to movements like Black Lives Matter have been vandalized, painted over, and removed after receiving backlash or through political pressure. In some cases, city officials have justified the removals by citing noncompliance with local ordinances or “divisiveness,” ignoring the reality that these images provide our communities with powerful affirmations of identity and solidarity.
Indigenous communities have faced similar symbolic erasure through the renaming of landmarks and suppression of their time-honored cultural practices. In some places in the States, school districts have banned Native regalia at graduation ceremonies using the argument that it conflicts with dress codes and willfully disregarding its deep- rooted significance. Still more, attempts to preserve monuments or language programs are frequently met with bureaucratic pushback, labeling these cultural expressions as “nonessential.” These moves are never one-and-done. They’re the first steps in a broader rolling back of visibility and voice. What starts with paint or policy often crescendos into something much much louder – unless communities recognize the signs early and step up .
Hillary Clinton recently sounded the alarm over the future of same-sex marriage in the United States, warning that the Supreme Court may soon “return the marriage issue to the states,” much like it did with abortion. In a stark comment that has since echoed across Queer advocacy circles both on and offline, Clinton advised LGBTQI+ couples to “get married now.” Clinton explained, “I don’t think they’ll undo existing marriages, but I fear they will undo the national right.” Her statement spotlights the sobering reality that rights once considered settled are no longer secure. Clinton is not simply politically forecasting here. In a way, she is calling us all to action, urging LGBTQ+ folks to safeguard what we can. Clinton’s words mirror a growing recognition that removing symbols – this time being our rainbowed crosswalks – tend to usher in judicial reconsiderations.
Meanwhile, Kim Davis – the former Kentucky county clerk who went to jail in 2015 for refusing to issue marriage licenses to same-sex couples – has petitioned the Supreme Court to overturn Obergefell v. Hodges. Davis, Represented by Liberty Counsel, argues that the landmark ruling is grounded in a flawed doctrine of substantive due process and describes it as a “legal fiction.” Liberty Counsel asserts that her First Amendment rights to religious freedom and free exercise were unjustly penalized, asserting that she should not have faced contempt, imprisonment, and a substantial monetary judgment just for simply “acting on her beliefs.” So this is where we are at.
In 2025, a sweeping wave of anti-LGBTQ+ policies has wrapped its talons around multiple levels of government, significantly lessening protections and visibility for queer and trans communities in our country. At the federal level, the Trump administration announced that starting in 2026, gender-affirming care will no longer be covered under the Federal Employees Health Benefits and Postal Service Health Benefits programs, affecting thousands of transgender federal workers and their families. Meanwhile, the Department of Education has labeled several Northern Virginia school districts, including Fairfax, Arlington, and Loudoun, as “high-risk” due to their upholding of inclusive policies for transgender students. These districts must now front over $50 million in education funding.
At the state level, hostility toward LGBTQ+ rights has swelled. More than 700 anti-LGBTQ+ bills have been introduced or passed in 2025 alone, targeting everything from flag displays to healthcare access. In Utah, Pride flags are now banned from government buildings, with daily fines imposed for noncompliance, while funding for Pride events has been drastically reduced. Nowhere is this oppressive legislative surge more aggressive than in Texas, where over 200 anti-LGBTQ+ bills have been introduced, including measures to restrict gender-affirming care, erase gender identity from official records, censor LGBTQ+ topics in schools, and redefine legal sex in rigid binary terminology. Stacked up, these developments represent a coordinated campaign to reverse decades of progress.
What can we do? First, we have to stay engaged. For starters, stop telling people that the news is too depressing to watch and find an outlet or three that resonate. Also, attend city council meetings, demand transparency from elected officials, and hold leaders accountable. Push for alternative expressions of support (public art, monuments, the whole gamut) that preserve the spirit of inclusion even when laws change.
Ultimately, we must amplify visibility. At a time in our country’s story where silence is easily mistaken for obedience, communities must get louder than ever in affirming their values. Take photos, tag photos, share stories, and call out those in places of power. Our rainbow crosswalks may be dropping like soldiers but the people they represent are still standing. Despite this bleak climate, WorldPride 2025 was held in Washington, D.C., doubling as both a queer-centric celebration and an indisputable act of protest against these escalating threats. Let’s keep that energy going, shall we?
In the end, what’s at stake is much greater than paint on pavement. It’s the affirmation that everyone deserves to be protected regardless of their identity. Let’s not wait until the last color is washed off our streets. Let’s repaint and resist. Let’s reimagine a country where all of us belong, every shade on that rainbow we hold so dear. We’re not red, white, and royally f*cked quite yet. Let’s make sure we never are.
-

 LGBTQ+ RESOURCES4 days ago
LGBTQ+ RESOURCES4 days agoHope on the other side: How Rainbow Railroad rescues LGBTQI+ people at risk around the world
-

 Movies3 days ago
Movies3 days agoIntensive ‘Riefenstahl’ doc dives deep into a life of denial
-

 Features24 hours ago
Features24 hours agoHarnessing identity: Mr. CMEN Leather 2025 bares his heart and soul
-

 AIDS and HIV5 days ago
AIDS and HIV5 days agoCommunity is the cure: AIDS Walk LA returns to fight HIV and funding cuts
-

 COMMENTARY5 days ago
COMMENTARY5 days agoFrom rhetoric to persecution: When the State labels trans people as terrorists
-
 Books3 days ago
Books3 days agoThese four intertwined stories will leave you flabbergasted
-

 Features5 days ago
Features5 days ago“Small is all”: L.A. Councilmember Ysabel Jurado discusses “small” but impactful moments of queer joy and political victory
-

 Events21 hours ago
Events21 hours ago“We are glimmers of hope”: LGBTQ+ advocates deliver powerful speeches defending queer rights at Equality Awards
-

 Miscellaneous24 hours ago
Miscellaneous24 hours agoTiffany ‘New York’ Pollard Dishes on queer storytelling in her new show ‘Slayers: Wheel of Fate’
-

 National3 hours ago
National3 hours agoLGBTQ rights on the line: What to watch as Supreme Court’s new term begins

