Gilead: More than Medicine
Gilead Sciences initiative breaks down health equity barriers in triple-negative breast/chest cancer diagnosis & treatment for Black women
Although the initial diagnosis is both challenging & devastating, many patients will survive & thrive, joining the other over four million breast/chest cancer survivors

By Edwina Eyre | WASHINGTON – Breast/chest cancer is the most common cancer among women, and a staggering 297,000 women in the U.S. are predicted to receive a breast/chest cancer diagnosis in 2023.
Although the initial diagnosis is both challenging and devastating, many patients will survive and thrive, joining the other over four million breast/chest cancer survivors in the United States. However, for women with triple-negative breast/chest cancer (TNBC) – particularly Black women – this landscape looks markedly different.
TNBC stands out as the most aggressive form of breast/chest cancer, offering limited treatment options and often spreading throughout the entire body by the time of diagnosis. Catching and treating the cancer early is critical, a task that’s made more daunting as TNBC is predominantly diagnosed in younger and premenopausal women.
Amidst these already formidable odds, Black women face even greater disparities for this cancer, and are three times more likely than white women to receive a TNBC diagnosis with significantly higher mortality rates than other racial and ethnic groups. Even further, Black women are more likely to be diagnosed with TNBC at a later stage, which complicates the prospect of a successful treatment.
The factors contributing to these inequities are rarely included in conversations around breast/chest cancer health outcomes. Research suggests that these disparities are caused by the impact of lived experiences of structural racism on the body, while others point to genetics. However, most analyses agree that structural healthcare barriers impede Black women from accessing adequate testing, treatment and care.
To expand conversations around TNBC and its impact on Black women, Gilead Sciences launched the Toward Health Equity for Black People Impacted by TNBC grant program in 2021 to help advance Black health equity across the cancer care continuum. Since its launch, Gilead has awarded $5.7 million to 21 organizations focused on supporting Black women and building capacity of Black-led breast/chest cancer organizations across the United States.
One of these organizations is SHARE Cancer Support, a national non-profit providing free resources, education and support to those diagnosed with breast/chest, ovarian, uterine and cervical cancer. To increase public knowledge around TNBC and Black women, SHARE recently hosted a series of focus groups analyzing the diagnosis and treatment experiences of Black women living with TNBC to help identify resources that dismantle existing barriers to care. SHARE hired two Black researchers to lead the study: Dr. Tisha Felder, Associate Professor at the College of Nursing at the University of South Carolina and Dr. Lucy Ingram, Professor and Department Head in the College of Public Health at the University of Georgia.
“Before anybody is even diagnosed, existing inequalities filter what experience any patient is going to have, especially for Black people in this country,” says Dr. Felder. “Providers need to be more educated about TNBC in Black women, and we need to make sure we are tailoring care to the needs of the people who are experiencing the issues.”
To understand the nuances of a TNBC diagnosis experience for Black women, Dr. Ingram and Dr. Felder spoke with 20 Black women to get a better understanding of their TNBC journey. The results were eye-opening: most of the women they spoke with had never heard of TNBC before their diagnosis. Furthermore, there were several instances where healthcare providers dismissed symptoms, despite some patients having a family history of cancer.
Typically, research findings like these remain confined to academic papers, but SHARE Program Director Megan-Claire Chase, who is also a breast cancer survivor herself, quickly spearheaded the creation of a TNBC info card and video series based on Dr. Ingram and Dr. Felder’s findings.
“What’s great about our partnership is that we aren’t waiting for the work to trickle down to those that need it,” said Dr. Felder. “SHARE is taking the findings we have right now and using them immediately. They’ve developed materials tailored specifically to Black women, ensuring that people benefit from this work sooner rather than later.”
Gilead’s support for SHARE goes beyond the funding of this project. “It’s unprecedented for a funder to be as engaged in connecting grantees as Gilead has been. It truly reflects that advancing health equity must be a collaborative effort,” Chase adds. “We all bring unique skills to the table, ensuring that we keep these women alive and empower the general public and Black community to ask questions and advocate for themselves.”
SHARE’s work with Dr. Felder and Dr. Ingram has laid a strong foundation, filling critical gaps and informing material development. “Having this research available validates the Black experience,” said Chase. “It’s proof that we’re not just being overly sensitive—it’s a fact that we’re often dismissed, a huge obstacle in trying to be heard and understood. It’s a call to action and education. These women aren’t just patients dealing with Triple Negative—they’re Black women. That extra layer of identity brings a whole set of unique challenges during treatment, making a real impact on their experience with diagnosis and care.”
Gilead: More than Medicine is part of a paid year-long collaboration between Gilead Sciences and the Los Angeles Blade
Gilead: More than Medicine
Breast Cancer Awareness Month: Louisiana’s largest cancer center is bringing care to you
According to Dr. Constance Cole Blunt, medical oncologist and medical director of cancer prevention and outreach at Mary Bird Perkins Cancer Center in Baton Rouge, the best way to get people to screen for cancer is by participating in its Prevention on the Go program.
In Louisiana, where cancer rates clock in at over 40% higher than the national average, this approach isn’t just innovative – it’s necessary. Too often in Louisiana, cancer is caught at an advanced stage, drastically limiting options for care and treatment. Breast cancer is the second most diagnosed cancer in the state and has a particularly devastating impact – although Louisiana is ranked 28th in the nation for breast cancer incidence, the breast cancer mortality rate in the state is the second greatest in the country.
The factors driving these statistics are complex and interwoven with the daily struggles many Louisiana residents face in accessing medical care. Many don’t have adequate insurance and are unable to stay up-to-date on regular physicals and medical check-ups, let alone receive comprehensive cancer screenings. Rural communities struggle with transportation to far-away medical centers and a lack of access is compounded by a lack of awareness about prevalent cancers, symptoms and risk factors. These challenges are even more pronounced for communities of color in the state, who face higher rates of poverty and lower rates of health insurance coverage compared with their white counterparts. Alarmingly, Black women in Louisiana are diagnosed more frequently and are more likely to die from breast cancer than the national average.
As the largest cancer care organization in Louisiana, Mary Bird Perkins Cancer Center builds its approach around addressing the unique barriers faced by communities across the state. The center brings together medical oncologists, radiation oncologists and strong partnerships with clinics and hospitals to deliver comprehensive cancer care and treatment to patients – all under one roof. Patients are supported by navigators who ensure they are referred to the appropriate mobile clinics and screening services in their own communities, and that high-risk patients are prioritized for doctor visits and have a plan for accessing them. Beyond medical treatment, patients grappling with a cancer diagnosis also have access to a full support system within the center, including a palliative care specialist to help manage pain, a therapist to support mental health during treatment and even a dietitian to ensure that they’re able to maintain a healthy diet outside of their treatment program.
“We want patients to be able to walk through the door – whether it be to manage a breast cancer diagnosis or to get a screening – and get the entirety of their care taken care of in this one location,” says Dr. Blunt. “For a state where we know funding, resources and access are limited, having a patient be able to access a one-stop-shop to manage their treatment definitely makes the burden of cancer care easier for them.”
However, when breast cancer is diagnosed at a later stage, even the most comprehensive treatment plan offers limited hope for a cure. That’s why Mary Bird Perkins is focused on going beyond treatment to address the problem at its root by expanding early detection and prevention efforts across the state.
In 2002, Mary Bird launched Prevention on the Go, a program designed to bring education and early detection services to locations where people live, work, worship, shop and play. As part of the program, Mary Bird drives their mobile clinic across the state, parking everywhere from church parking lots to workplaces and creating what Dr. Blunt calls a “low intimidation environment” where people can connect with healthcare providers in a familiar setting. The events offer cancer screenings, but also health history reviews and education about preventive care. They also often provide activities, food and cooking demonstrations for community members.
“Our mobile clinics give information about detection and prevention to people in a way that’s easy to digest and fun,” explains Dr. Blunt. “Some patients come back and get their screenings with us, but sometimes these events just jumpstart somebody’s health journey. Both are important.”
Hematology, Medical Oncology
(Photo: Mary Bird Perkins Cancer Center)
For Dr. Blunt, Mary Bird Perkins’ mission is personal. When she was in undergrad, her mother’s best friend passed away from advanced ovarian cancer — her first exposure to both cancer and hospice care.
“You don’t forget experiences like that,” says Dr. Blunt. “She was a working mom who gave everything to her children but had gone years without getting any cancer screenings. By the time her cancer was caught, it was very advanced.”
Mary Bird Perkins’ programming has made huge progress toward ensuring that these types of stories are less common. Since 2002, Prevention on the Go has provided more than 118,000 screenings in local communities and detected nearly 900 cancers. As a testament to their important work, Mary Bird Perkins is a recipient of Gilead Sciences’ Oncology Grant Program, an initiative aimed at advancing health equity for people impacted by cancer. In 2024, Gilead announced an overall commitment of $5 million in grant funding, spread across a number of different organizations, to support additional health equity programs globally. To date, it has awarded more than $18 million in health equity-related oncology grants for programs that advance health equity for disinvested communities.
This support has been integral in helping Mary Bird Perkins expand their Prevention on the Go efforts and expand their overall programming. “In cancer care, collaboration is really important,” Dr. Blunt emphasizes. “The more stakeholders we have at the table, the more resources we have. Partnerships help us improve access, make sure our technologies are up to date and continue to provide great care to the communities that need it. Support from organizations like Gilead allows us to put patient care first.”
AIDS and HIV
National Latino AIDS Awareness Day: Breaking down stigma, silence and silos
FLAS provides HIV and STD education

When Elia Chino, Founder and Executive Director of the Fundacion Latinoamericana De Acción Social (FLAS) Inc., initially approached major HIV/AIDS agencies in Houston, Texas for support in starting an organization tailored specifically to reaching Latino populations, she was met with confusion.
“Why do you want to start a separate organization?” they asked. “We’re here!”
Chino remembers her frustration. “They didn’t understand,” she said. “Our brothers and sisters were dying, and the community needed services that they couldn’t provide.”
Indeed, in the 1990s, barriers to HIV care and treatment for Latino populations were markedly different from those faced by other populations. Information about the HIV epidemic was largely in English, and inaccessible to many individuals who had immigrated from indigenous Latin American communities and never learned to read and write in their native language, let alone English. When they were able to access treatment, Latino individuals often faced mistreatment at primary care facilities due to a lack of culturally competent care.
Perhaps most challenging was the culture of silence. Many Latino immigrants living with HIV in the United States fled homophobia, transphobia and stigma in their home countries, and were still grappling with lasting shame and guilt. Despite many people dying, there was little open discussion or education about the cause. In fact, Chino didn’t even know that the HIV epidemic took the lives of some of her best friends until speaking with their families years later.
“No one was talking about their diagnosis,” says Chino. “People had come to the United States for freedom, but still weren’t ready to talk about who they were. There was a real atmosphere of stigma, taboo, misinformation and fear.”
At the time, Chino was volunteering at a hospital serving communities without insurance. The fourth, fifth and sixth floors were all dedicated to treating people with HIV. Chino began educating herself on this crisis while she volunteered at the hospital, and founded FLAS in 1994 after discovering that the majority of HIV prevention efforts were not reaching Latino individuals.
In the beginning, without support from other organizations in the area or resources to expand, Chino was a one-woman show, conducting outreach in clubs, cantinas and bars by herself. She hadn’t anticipated the barriers she’d face as a member of the LGBTQ+ community and an immigrant. Horrible discrimination, a language barrier and intense HIV stigma in the communities she was working in made the work challenging, but also emphasized the necessity of what she was doing.
Over time, with support and funding from organizations like Gilead Sciences, FLAS has been able to expand its services from solely HIV prevention to include HIV testing, behavioral health services, housing and social services assistance, support groups and a food pantry. The organization has started hosting educational events everywhere from churches to street corners, raising awareness about HIV in the Houston community. Chino also started collaborating with the consulate of Mexico to help newcomers navigate U.S. health systems and services when they arrive in the United States. Next year, the organization will start offering mobile HIV testing clinics for communities in need.
Since its launch, FLAS has been able to expand its initial focus to address the holistic drivers of this crisis, moving beyond medical determinants of health to tackle the social and structural barriers that perpetuate the HIV epidemic and prevent Latino populations from accessing comprehensive treatment.
“Everyone keeps telling Latino individuals to get tested, but this does nothing unless you actually incentivize people to do so,” says Chino. “People have to go to work. They have to pay their rent. They have to buy food. Many can’t afford to lose their salary and spend a full day coming in to do a test or get treatment. We have to make it easier to access HIV prevention and treatment, and we have to provide incentives.”
This year marked FLAS’s 30th anniversary, which the organization celebrated with a gala in August. They have made a huge impact in Houston since their launch – providing HIV and STD education to over 500,000 Latino people, distributing over 20,000 HIV tests, referring over 40,000 people for social services and hosting over 6,000 educational events and health fairs in English and Spanish. However, many of the challenges for HIV prevention and treatment for Latino populations remain.
“We have over 30,000 individuals living with HIV in Houston, yet when we ask for people to talk about their status, no one comes forward to tell their stories. HIV is a chronic disease, but stigmatization is still so strong in the Latino community,” says Chino. “You can say you have cancer, high blood pressure, diabetes, whatever – but nobody says I have HIV. There is still so much work to do.”
As a testament to their important programming, FLAS is a recipient of funding through Gilead Sciences’ TRANScend® Community Impact Fund, a program aimed at empowering Trans-led organizations working to improve the safety, health and wellness of the Transgender community. Since its inception in 2019, TRANScend has awarded more than $9.2 million in grants to 26 community organizations across 15 U.S. states and territories.
TRANScend support has been critical to helping FLAS maintain its services. In 2020, in the midst of the COVID pandemic, Gilead’s funding helped FLAS continue to offer virtual behavioral and mental health services to the community when their physical offices had to close.
According to Chino, this type of partnership is critical to ending the HIV epidemic in Latino communities, especially for meeting communities where they are.
“Communities trust their grassroots organizations, and grassroots organizations provide for their communities,” she says. “At the end of the day, we need to continue to support the groups doing the difficult work on the ground with the people they’re serving, especially those breaking down stigma and lasting barriers to care for Latino communities.”
Gilead: More than Medicine
Gilead and the Community Education Group are centering Appalachian voices at USCHA
Community Education Group Founding Executive Director A. Toni Young likes to say that her organization works from the ‘hood to the holler’ when it comes to HIV prevention in the U.S. South. Since its launch in 1996, Community Education Group has worked to break down lasting barriers to care and treatment for HIV and other prevalent sexually transmitted infections in communities ranging from the “hoods” of urban southeast D.C. to the “hollers” of rural West Virginia.
Last week, Young and her team took their work on the road to New Orleans, Louisiana, for the United States Conference on HIV/AIDS (USCHA), the largest conference for HIV in the country. The event convenes thousands of stakeholders from all levels of HIV prevention and education efforts to discuss priorities for tackling the root causes of the ongoing HIV epidemic. This year, Community Education Group used USCHA to identify new solutions for combating rising HIV rates in Appalachia, a region currently experiencing an alarming spike in diagnoses as a result of the opioid epidemic.
“Picture a train roaring through Appalachia,” says Young. “The engine is the oxycontin crisis, which has devastated the region for years. The cars on that train are Hepatitis C, B and A, educational attainment challenges, workforce development challenges, and economic struggles. The caboose is the HIV epidemic. These factors work in tandem, perpetuating and exacerbating each other.”

In 2025, Community Education Group at Healing Appalachia hopes to test 2,500 people at Healing Appalachia to sup5ort Appalachian communities impacted by substance use disorder. (Photo provided by Community Education Group at Healing Appalachia)
Despite bearing the burden of this crisis, Appalachian communities are often excluded from more extensive conversations around HIV, hindering efforts to effect real change in the region. Rural providers have long been focused on the oxycontin epidemic and have only recently begun to grapple with the resulting HIV outbreak on the scale that urban communities have been addressing since the 1980s. This lag has led to a widespread lack of awareness about the epidemic in the region, and the response has typically been siloed.
To address these awareness gaps, Community Education Group, with support from Gilead Sciences, offered scholarships covering registration, lodging and travel for 30 individuals from rural Appalachian communities to attend and participate in USCHA. These participants, ranging from regional healthcare providers to people living with HIV themselves, were able to attend sessions on prevention, care and treatment options while meeting with other people living with and impacted by HIV and, most importantly, engage in crucial conversations about HIV prevention for their communities.
The key takeaways from these discussions centered on two main goals for the coming years: 1. ensuring individuals know their HIV status, and 2. helping them understand and access available treatment options, including learning the latest science of prevention, care and treatment. However, these conversations also elucidated that both goals will be difficult to accomplish unless local strategy acknowledges and addresses the specific circumstances of each individual they’re trying to reach and the unique barriers to care that they might face.

Community Education Group Founding Executive Director A. Toni Young. (Photo courtesy Community Education Group at USCHA)
“What worked for white gay men in San Francisco is not necessarily going to be what works for people impacted by substance use disorder in rural West Virginia,” says Young. “We can’t only ask whether someone has HIV. We need to identify and address the structural factors that might affect their ability to get tested and treated, like workforce opportunities, education and housing. It is critical that we take a syndemic approach, addressing HIV, HCV and substance use disorder.”
This intersectional approach has been the crux of Community Education Group’s recent work. In March 2022, the group launched its Appalachian Partnership Fund, which supports sixteen local groups addressing HIV, Viral Hepatitis and substance use disorder in West Virginia’s most vulnerable and rural populations. In addition to the Partnership Fund, Community Education Group hosts monthly calls with regional leaders in the HIV, HCV, STI and substance use disorder space who provide valuable information about local care and treatment options. Additionally, the organization recently began its Community Health and Medical Personnel Services (CHAMPS), an educational program designed to build further awareness of HIV and hepatitis C with community health workers in Appalachia, and train them on harm reduction skills and tactics.
Young emphasizes that while Community Education Group works to strengthen provider networks and implement harm prevention solutions, the group’s programming is focused on building relationships with the community above all. They encourage individuals to contact them with questions about anything from HIV treatment to where to get a free turkey for Thanksgiving, which helps build trust between the community and regional healthcare providers and makes it easier for Community Education Group to serve as a resource when needed.
Support from Gilead Sciences has been crucial in this work. According to Young, Gilead centers the voices of on-the-ground experts and supports them in executing their own visions for what will make the most impact for the communities they work with.
“Gilead really understands the wholeness of who I am as an individual and as a leader,” says Young. “They understand the wholeness of the organization and the wholeness of the people we serve. We can’t function as an organization or make any tangible impact on barriers to HIV care and treatment in the region if we don’t see people as all of what they are. Gilead really recognizes that, and that support is what allows me, a dreamer, to implement our mission and vision bringing resources, opportunity and attention to the people of the Appalachian Region to address the HIV, HCV and substance use crisis.”
Gilead: More than Medicine
Gilead announces new phase in partnership with Elton John AIDS Foundation
Effort to address barriers to HIV care, treatment in Eastern Europe and Central Asia

This month, Gilead announced the next phase of its partnership with the Elton John AIDS Foundation (EJAF) through RADIAN®, a program aimed at addressing HIV rates in Eastern Europe and Central Asia (EECA). The extended partnership will continue meeting the evolving needs of the most vulnerable key populations in the region, including people who use drugs, men who have sex with men, sex workers and Transgender individuals.
RADIAN works directly with grassroots organizations and partners in EECA to address HIV-related challenges in the region. Since its launch in 2019, RADIAN has reached over 271,000 people with HIV services, reinitiated or initiated over 26,500 people on antiretroviral therapy, trained more than 14,000 frontline workers to reduce stigma and discrimination and provided more than 114,000 HIV tests.
Although the program has spurred concrete progress, EECA is still in crisis – it is one of the few regions in the world where the HIV epidemic is getting worse, with new HIV diagnoses and AIDS-related deaths increasing by 20% and 34%, respectively, since 2010. The conflict in Ukraine has caused mass displacement, and the disruption of healthcare services, an increase in anti-LGBTQIA+ legislation, stigma and discrimination are greatly hindering the HIV response.
To address remaining barriers to care and treatment, Gilead is doubling down on its commitment to tackle HIV in the region through the next phase of RADIAN. Over the next five years, Gilead will commit $25 million to further support collaborative, community-based action to help end the HIV epidemic in EECA.
During this next phase of the partnership, RADIAN will expand its geographic reach to support key populations, particularly migrants and refugees, affected by and fleeing the conflict in Ukraine, launch an “innovation fund” to increase the effectiveness of the HIV response in EECA by supporting emerging innovations on a rolling basis, replicate and disseminate successful models and projects from the ‘Model Cities’ program to help close gaps in HIV prevention, testing and treatment and continue to address structural drivers of the epidemic to strengthen HIV health systems and build the capacities of local organizations.
Gilead: More than Medicine
Gilead’s HIV Age Positively® grant program spotlights unique needs of individuals aging with HIV
On September 18, healthcare providers, advocacy organizations, and communities across the country will commemorate National HIV/AIDS and Aging Awareness Day
By Edwina Eyre | WASHINGTON – While HIV was once considered a death sentence, major medical breakthroughs coupled with advancements in HIV prevention education and stigma reduction have transformed the virus from a once-fatal disease to a chronic condition that can allow individuals to live long and healthy lives.
Today, more than half of the adults living with HIV in the U.S. are over 50 years old. By 2030, that number will jump to 70% – a number that was unimaginable 30 years ago. While this transformation is a tremendous step forward, it has ushered in its own set of challenges when supporting this new, aging population that has distinct care and treatment needs.
On September 18, healthcare providers, advocacy organizations, and communities across the country will commemorate National HIV/AIDS and Aging Awareness Day (NHAAD) to raise awareness of the impact of HIV/AIDS on older Americans, and the urgent need to expand testing, treatment and care services for individuals over 50.
By 2030, more than 80% of people living with HIV will have at least one age-related medical condition, such as cancer or heart disease. Individuals living with HIV may also contend with various comorbidities that intersect with their diagnoses, such as diabetes, liver disease, anemia and high blood pressure. They may also face a different set of psychological and mental struggles than their peers.
However, few dedicated resources exist to address the diverse needs of the growing population of older individuals living with HIV. “HIV services and aging services have historically been very siloed,” says Prescott Chow, Director and Co-Principal Investigator for the Training and Health Equity (T.H.E.) Collaborative at the University of California, San Francisco. “While there have been some touchpoints, there have also been a lot of missed opportunities in terms of figuring out how to develop services that are inclusive of folks who are aging with HIV.”
The lack of attention and funding for the rapidly increasing population of individuals over 50 living with HIV prompted Gilead Sciences to launch HIV Age Positively® in 2018, an initiative aimed at supporting programs focused on improving the quality of life and health for those who are aging. Since its launch, the program has awarded more than $35.8 million in grants to support 42 organizations — from healthcare organizations to advocacy groups working to address the interrelated challenges within the healthcare system and the general HIV community — addressing stigma, loneliness and better coordination of care.
HIV Age Positively centers on three pillars: (1) improving care coordination, (2) increasing resources for better well-being and (3) educating and informing policy related to aging with HIV. Grantees work to provide resources such as mental health services and community support and make sure people aging with HIV receive the care they need by training and educating healthcare professionals with additional literacy around HIV and comorbidities.
T.H.E. Collaborative, an HIV Age Positively grantee, provides capacity building, technical assistance and training services to other grantees across a 13 state region in the Western U.S. In addition to HIV Age Positively grantees, T.H.E. Collaborative frequently works with other HIV advocacy programs in the Western U.S., providing a platform for peer-to-peer support and training.
“We are currently in this new era in aging, where we are really looking at the whole person and focusing on intergenerational and intercommunal care,” remarks JB Del Rosario, the Care and Wellbeing Center Project Manager at T.H.E. Collaborative. “So much of this work is about paying it back, but also paying it forward – recognizing the work that people who have come before us have done, but also passing on that effort to the coming generation as well and taking the lessons that we’ve learned to create a better world and a better system.”
One of the ways T.H.E. Collaborative is centering intercommunal HIV and aging care is through their Collaboration in Care Conference. On September 18 and 19, an interdisciplinary network of more than 200 providers from both the aging and HIV space will come together in Sacramento, California, to share best practices from their work and different resources available in their fields. Participants will cover topics as varied as financial health, mental health, community building and the psychosocial aspects of aging with HIV.
Del Rosario and Chow were thrilled to have T.H.E. Collaborative’s work, including the Collaboration in Care Conference, supported by Gilead through HIV Age Positively and emphasized the need for continued focus on wraparound care to address the health needs of those aging with HIV.
“It feels like a gift right now to think about how to look at HIV differently,” says Chow. “Where we are now is amazing in terms of the biomedical interventions we have available to help people aging with HIV have healthy long lives, but with that comes the responsibility to consider the other issues that impact a person’s life and to ensure that individuals are not just surviving but thriving as they age with HIV.”
Gilead: More than Medicine is part of a paid year-long collaboration between Gilead Sciences and the Los Angeles Blade
Gilead: More than Medicine
Inaugural #ZeroHIVStigmaDay leaders urge us to see one another as human
Zero HIV Stigma Day was chosen to honor Prudence Nobantu Mabele, the first South African woman to disclose her HIV status in 1992

By Donovan Harris | WASHINGTON – There is something powerful about embracing our shared humanity.
For leaders and activists in HIV care and prevention, that is the message they are working hard to spread in the fight against HIV-related stigma.
“I’m stunned that some of the same stigma that we experienced in the early days of the epidemic continues to persist and are so pervasive across society,” said José Zuniga, president/CEO of the International Association of Providers of AIDS Care (IAPAC).
Zuniga was open about his experiences as a Gay, Latino man, sharing that he is no stranger to the deep-rooted stigma millions of others in the LGBTQ+ community experience.
“I clearly understand the stigma that comes with people judging us based on our sexual orientation,” he said. “There’s a self-stigma, the self-labeling and the [fear] of feeling unworthy or being othered.”
Zuniga expressed that he is disheartened that HIV-related stigma extends to some healthcare settings, causing many people to delay essential, life-saving care. “It only takes one person within the healthcare system to stigmatize you before you hesitate to do what should be done to mitigate your risk, either becoming HIV positive or progressing to AIDS if you’re newly diagnosed with HIV,” he said.
According to UNAIDS, people living with HIV who perceive high levels of HIV-related stigma are 2.4 times more likely to delay enrollment in care until they are very ill.
However, there has been progress globally to reduce stigma and provide greater access to HIV care. In a recent UNAIDS report, researchers found there is a clear path to ending AIDS by 2030. Botswana, Eswatini, Rwanda, the United Republic of Tanzania and Zimbabwe have already achieved the “95-95-95” targets.
The goal is for 95% of all people living with HIV to know their HIV status, 95% of people diagnosed with HIV infection to receive antiretroviral treatment and 95% of people who are being treated are virally suppressed by 2025.
While we have seen notable strides over the years, Zuniga said more work must be done to reduce HIV-related stigma globally.
That is why he is proud of the work done to launch the inaugural Zero HIV Stigma Day on July 21, 2023. The day was chosen to honor Prudence Nobantu Mabele, the first South African woman to disclose her HIV status in 1992.
“There was no awareness day singularly focused on stigma,” Zuniga said. “There certainly is one [day] around discrimination, but discrimination is really an outcome of stigma.”
Zero HIV Stigma Day was announced in 2022 as a collaboration between the IAPAC, a UK-based sexual health charity called NAZ, the Global HIV Collaborative and the Fast-Track Cities Institute.
Gilead Sciences also stepped in to amplify the important work Zuniga and his team are doing to end stigma on Zero HIV Stigma Day and throughout the year.
Through a grant from Gilead, Zuniga said his organization was able to implement one of the first medical education programs for primary care providers around “Undetectable=Untransmittable” which means a person cannot pass HIV through sex when they have undetectable levels of HIV.
He also said the pharmaceutical company was an early supporter of the Fast-Track Cities Institute and has helped reduce HIV-related stigma by providing resources and education through their COMPASS Initiative®, a 10 year, more than $100 million commitment to end the HIV/AIDS epidemic across the U.S. South.
“This is serious work and not something that any entity takes lightly,” Zuniga said.
This year’s Zero HIV Stigma Day theme is “Human First” to emphasize the humanity of people living with and affected by HIV.
“Pushing this human first message to us is critical because of course, the H in HIV stands for human,” Zuniga said. “I think we can repair the very frayed level of connectivity between us because we share a common humanity.”
Gilead: More than Medicine is part of a paid year-long collaboration between Gilead Sciences and the Los Angeles Blade
Gilead: More than Medicine
The new mission to fight HIV devastation in rural America
Black, Latino, Native American, and other minority groups residing in rural regions have higher than average rates of HIV
RIDGELAND, MS – Twenty years ago, Mississippi-based Dr. June Gipson was contacted by researchers who were conducting a study of Black men living with HIV over the age of 45 in Mississippi. They wanted a list of subjects with whom to talk. It should have been an easy assignment.
It wasn’t. There weren’t enough people to talk to. Vast numbers of Black men living with HIV in the state had died.
Decades later, thanks to missions like Dr. Gipson’s, improved medicines, and more knowledgeable wellness, that is no longer the case. There is a growing population who are living and aging with HIV.
“Essentially what My Brother’s Keeper does is training: we teach others what we do, we teach others how to sustain. We teach others how to work within the environment to be successful, “ Dr. Gipson told me.
Today, people living with HIV routinely live into their 50s, 60s, and beyond, but they still have needs that extend beyond the HIV challenges themselves. Especially in rural areas, there is isolation, stigma and poor mental health environments. Dr. Gipson leads an organization to give them resources and a deeper sense of wellness than they have ever imagined.
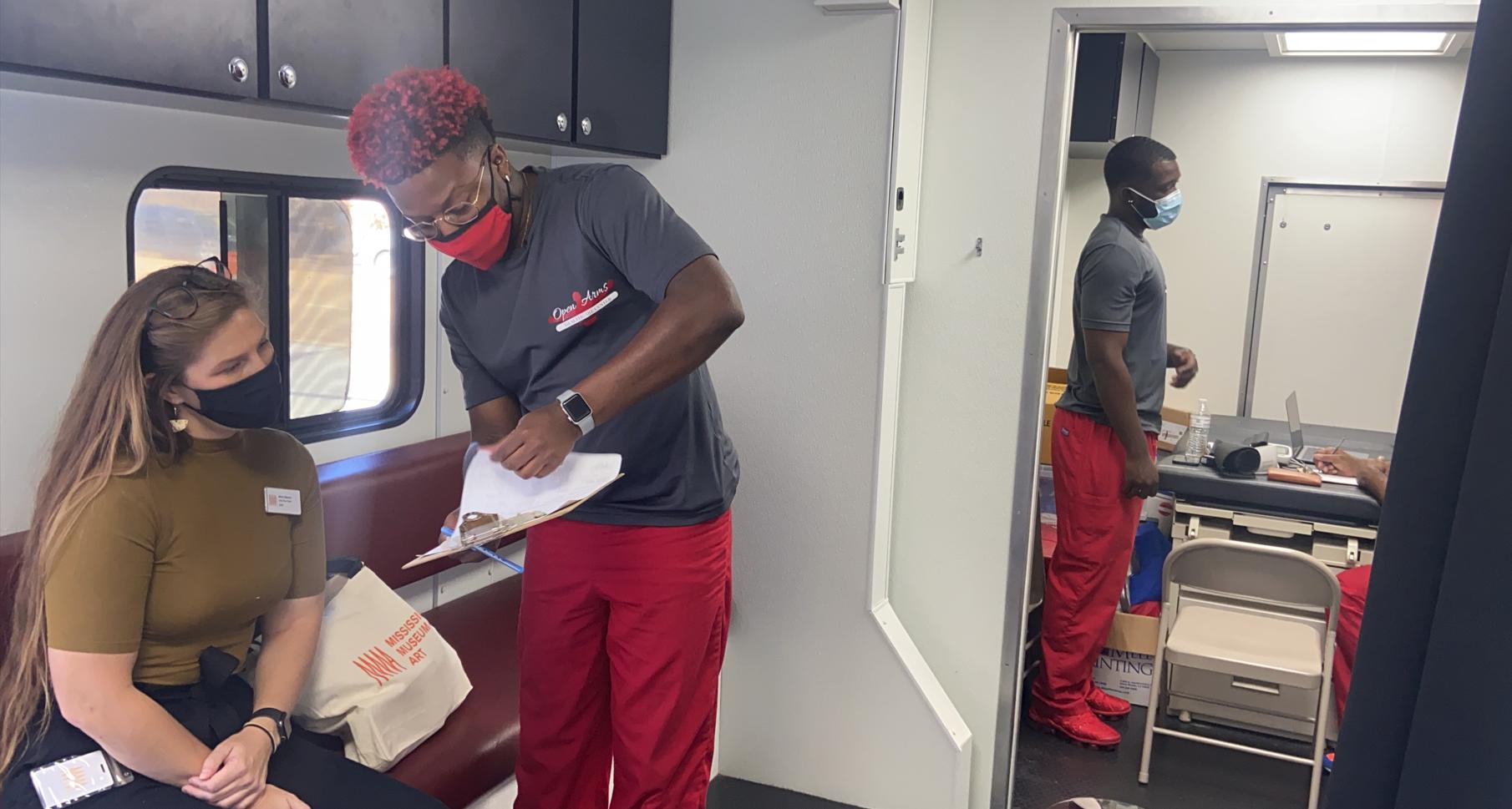
Dr. Gipson is the President and CEO of My Brother’s Keeper in Ridgeland, Mississippi. My Brother’s Keeper has expanded its service range into the clinical arena with the establishment of Mississippi’s first LGBTI primary healthcare clinic, Open Arms Healthcare Center. With a background that spans criminal justice and education in addition to healthcare, Dr. Gipson is a formidable leader and evangelist in creating effective and available healthcare in rural and marginalized communities. Her organizations not only provide services to such communities, they teach other organizations how to do the same. With a new grant from Gilead’s Zeroing In™ program — which aims to support organizations working to increase the overall health and wellness of communities most impacted by the HIV epidemic — they have been tapped to provide technical assistance and capacity building to other organizations.
Dr. Gipson’s advice to other organizations following the My Brothers Keeper/Open Arms model? “Just do it. When someone goes into the healthcare arena as a community-based organization, there’s a level of fear but… you’re going to have to just do it. You’re not going to have all the answers in the beginning. You will learn things along the way, but you do have to get started,” she says.
My Brothers Keeper and the Open Arms Healthcare center work synergistically to provide services to the community with an emphasis on the particular needs of LGBTQ individuals. “We have a wonderful avenue to not just do the work, not just teach others how to do the work, but to combine these things into real life lessons. We are the epitome of what community-based programs can become.” Dr. Gipson is in a constant state of continuous improvement. She is embarking on research with organizations in London and Australia to perfect best practices to reach out in underserved communities.
She acknowledges that such communities, especially the one she has served in Mississippi, are difficult to reach because accurate healthcare education is actively discouraged. “I think that the fact that we lack so much education around reproductive health and sex ed puts us at a complete disadvantage. The system is still talking about abstinence, which is not effective. We’re still bringing up abstinence when we have some of the highest HIV rates and some of the highest STI rates.”
Gilead is determined to make a difference. “We go where the need is greatest,” is a phrase they use frequently.
In this case, that “where” is in rural areas in the United States. These communities face disproportionate challenges in accessing HIV and other healthcare services caused by a shortage of local doctors, poverty, and remote locations. The patient-to- primary care physician ratio in rural areas is only 39.8 physicians per 100,000 people, compared to 53.3 physicians per 100,000 in urban areas. Additionally, 59% of the decline in the number of US community hospitals between 2015 and 2019 were rural hospitals and 47% of rural hospitals have 25 or fewer staffed beds. Seven states have a disproportionately high number of HIV diagnoses in rural areas: Alabama, Arkansas, Kentucky, Mississippi, Missouri, Oklahoma and South Carolina. In the U.S. South, 23% of new HIV cases happened in rural areas, and for late-stage diagnosis, the percentage for Black people was higher than in urban or metropolitan areas.
That was consistent with the fact that Black, Latino, Native American, and other minority groups residing in rural regions have higher than average rates of HIV.
In March, Gilead Sciences announced $3 million in grant funding to eight organizations through the Zeroing In grant program, including My Brother’s Keeper, to provide services to communities disproportionately impacted by HIV in rural areas in the United States. Darwin Thompson, Director of Public Affairs at Gilead Sciences stated at the announcement, “Our Zeroing In rural grants are helping organizations expand their testing programs, provide remote communities with access to necessary resources and fight ongoing stigma by promoting a culture of compassion and inclusion. We know it takes more than medicine to end the HIV epidemic for everyone everywhere. By supporting these organizations, we’re increasing their capacity to educate communities, change perceptions and provide critical access to healthcare where it’s needed most.”
Dr. Gipson and other leaders were selected for investment due to their strategic, community-driven approaches toward dismantling systemic barriers that prevent people in rural communities from accessing quality HIV testing and treatment.
“The funding from Gilead was a gamechanger. What Gilead gave us was the needed startup funds to be able to do this work. I remember opening my clinic. I remember, it was literally $8,000 that was separating me from opening. There were expenses for exam beds, cotton balls. Band-Aids – simple things that should not impede someone from starting a new business, but those were the pieces that held me back,” Dr. Gipson says of the Zeroing In project.
The project is designed to bring healthcare equity and stop HIV devastation in all venues. While HIV is prevalent in both urban and rural communities in the United States, resources are heavily concentrated in urban centers, and lack of public health infrastructure and heightened stigma in rural communities create barriers of access to necessary care.
As Dr. Gipson points out, Gilead and Zeroing In are dedicated to changing the game. My Brother’s Keeper and its sister grantees are literally keeping their fingers on the pulse of people living with HIV with dedication and determination.
Gilead is equally determined to see them succeed with wellness and health for all.
Gilead: More than Medicine is part of a paid year-long collaboration between Gilead Sciences and the Los Angeles Blade
-
 a&e features24 hours ago
a&e features24 hours agoQueer highlights of the 2026 Critics Choice Awards: Aunt Gladys, that ‘Heated Rivalry’ shoutout and more
-

 Television3 days ago
Television3 days agoThe ‘Stranger Things’ coming out scene: The reaction and the relevance
-
 Books4 days ago
Books4 days agoA look back at the best books of 2025
-

 LGBTQ+ Youth Mental Health4 days ago
LGBTQ+ Youth Mental Health4 days agoLaw expanding mental health resources for LGBTQ+ youth has gone under effect
-

 National22 hours ago
National22 hours agoTop 10 LGBTQ national news stories of 2025