Human health studies & sciences
Genetic variations linked to human bisexual behavior
Behavior, risk-taking, & offspring numbers uncovered in a study from Professor Jianzhi ‘George’ Zhang at the University of Michigan

ANN ARBOR, Mich. – In a groundbreaking study published Wednesday in Science Advances, scientists have identified genetic variations associated with human bisexual behavior for the first time.
Led by Professor Jianzhi “George” Zhang at the University of Michigan, the research delves into the intricate relationship between genetics, behavior, and societal factors, shedding light on the long-standing evolutionary puzzle of why natural selection has not eradicated the genetics underpinning same-sex attraction.
The study, based on data from more than 450,000 people of European descent who participated in the UK Biobank, a long-term genomics project, builds on growing research, including a seminal 2019 paper in Science that found genetic variants influencing same-sex behavior, with environmental factors playing a significant role.
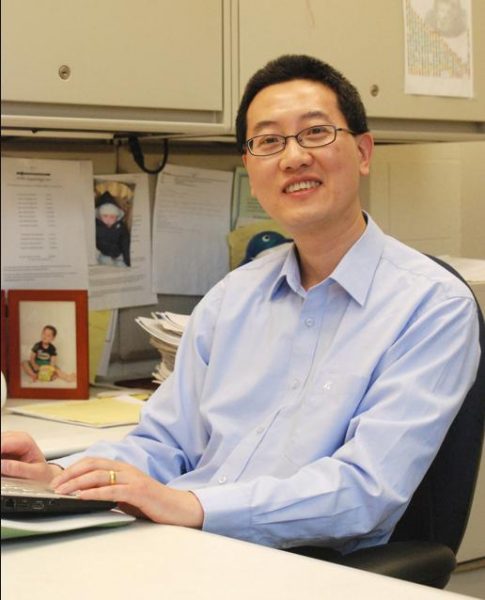
Zhang explained that the motivation for the new research was to differentiate between various forms of homosexual behavior, recognizing that there is a spectrum. “In the past, people lumped together all homosexual behavior…but actually, there’s a spectrum,” he said.
Analyzing participants’ complete sets of DNA and combining that information with survey responses, Zhang and co-author Siliang Song confirmed that the signatures associated with same-sex behavior and bisexual behavior were distinct. This allowed them to analyze these behaviors separately, leading to intriguing discoveries.
Male heterosexuals carrying markers associated with bisexual behavior (BSB)-associated alleles were found to father more children than average, suggesting reproductive advantages. Moreover, men identifying as risk-takers tended to have more children and were more likely to carry BSB-associated alleles.
“Our results suggest that male BSB–associated alleles are likely reproductively advantageous, which may explain their past persistence and predict their future maintenance,” the authors wrote.
Nature’s complexity was underscored by Zhang, noting that a single gene can influence multiple traits, a phenomenon known as “pleiotropy.” “Here we’re talking about three traits: number of children, risk-taking, and bisexual behavior—they all share some genetic underpinnings,” he said.
Exclusive same-sex behavior (eSSB) associated alleles, however, were correlated with having fewer children when carried by heterosexual men, indicating that these traits may diminish over time.
The UK Biobank data revealed a significant trend—the proportion of people reporting both bisexual and homosexual behavior has been rising for decades, likely due in part to growing societal openness.
In an additional report, scientists announced on Wednesday that they have identified genetic variations associated with human bisexual behavior. The study builds on the University of Michigan research and further emphasizes the link between these genetic variations and risk-taking behavior, as well as the impact on offspring numbers when carried by heterosexual men.
The authors of both studies estimated that approximately 40 percent of a person’s behavior regarding bisexuality is influenced by genetics, while 60 percent is influenced by the environment. Emphasizing the contribution to understanding human sexuality, the researchers stressed that their results are not intended to endorse discrimination based on sexual behavior.
This comprehensive research provides a nuanced perspective on the interplay between genetics, behavior, and societal factors in shaping human sexuality, opening the door to further exploration in this complex and evolving field.

Health
Breaking down the latest mpox vaccination survey results
The survey focused on the LGBTQ+ community of Southern California

Of the 255 people surveyed at Pride events throughout 2024, about 74% of respondents who have been vaccinated against mpox identified as gay, and of those, 41% identified as Latin American, 36% as White, and 18% as Black.
The California HIV Research Policy and Research Centers released the new survey this month, highlighting characteristics and prevention behaviors of Southern Californians who have been vaccinated against mpox.
According to the World Health Organization, mpox is an illness caused by the monkeypox virus. There are groups of organisms that share a common ancestor and all of its descendants, called clades. The virus has 2 distinct clades–clade 1 and clade 2, with both of those clades having a and b subclades. During 2022 and 2023, a global outbreak of mpox was caused by the clade 2b strain.
Today, mpox continues to be a threat globally, with cases caused by the clades 1a and 1b still surging in Democratic Republic of Congo and other countries, raising concerns.
The Blade spoke with Dr. Ian Holloway, researcher at the Southern California HIV/AIDS Policy Research Center, to get more details on the survey.
“We recently saw the first clade 1 infection in California, up in San Francisco,” said Dr. Holloway. “It was the first claude 1 infection in the United States and it happened up north, adding some additional urgency to this work.”
He further explained that though the recent infection in California added urgency to this work, the survey results had been collected over 2024, with specific focus on pooling vaccination data from Pride events across SoCal counties which include Los Angeles, Santa Barbara, Orange and San Diego.
Black and Latin American people are overrepresented in terms of mpox cases in Los Angeles County.
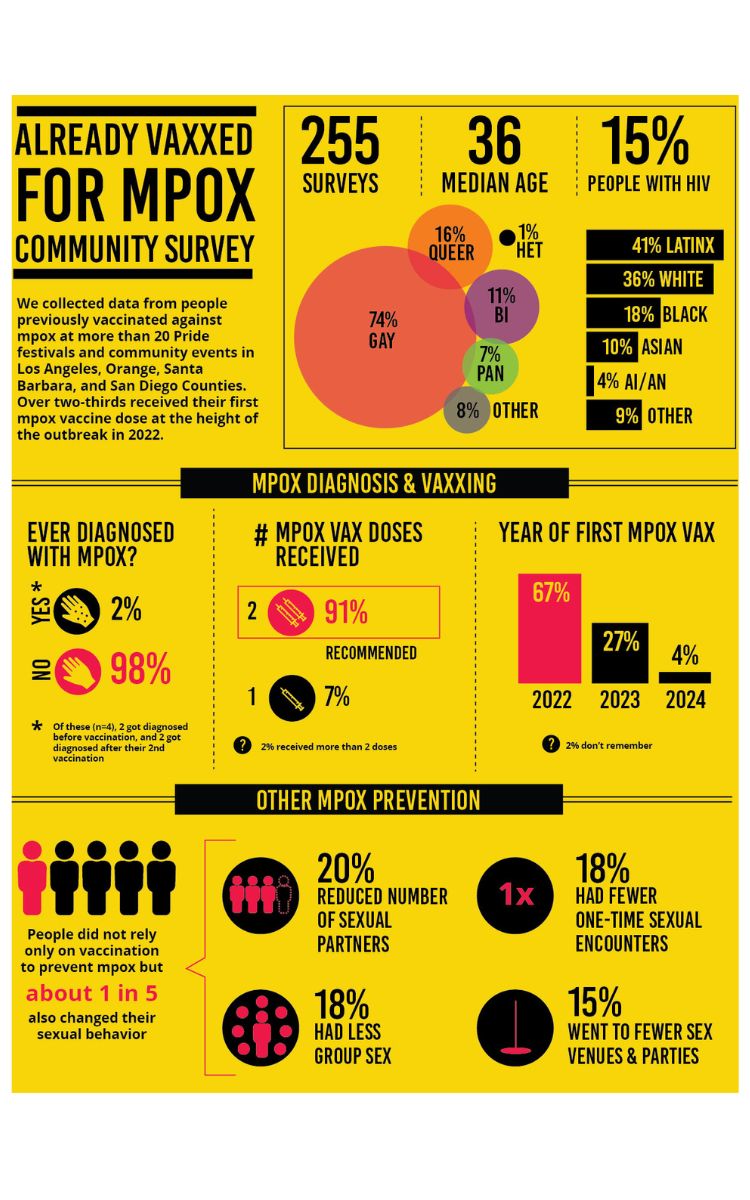
Infographic courtesy of the California HIV/AIDS Policy Research Centers
“There is a higher percentage of mpox cases among those groups, than their representation in the general population. They also have lower vaccination rates, compared to their White counterparts, so our efforts certainly highlight the need for culturally tailored and culturally relevant mpox education and community outreach materials in order to close the gap and provide more robust vaccine coverage, especially for Black and Latinx, queer people.”
The study found that 67% of those surveyed received the first of 2 mpox vaccine doses during the 2022-23 outbreak, with 91% of those having received both necessary doses. The survey also pointed out that people did not rely on vaccination alone to protect against mpox, because about 20% of respondents also reduced their number of sexual partners or made other behavioral adjustments to reduce the risk of contracting the virus.
To reduce the risk of infection, 20% of respondents reduced their number of sexual partners, 18% had less group sex, 15% attended fewer sex venues or parties, and 18% had fewer one-time sexual encounters.
The survey also noted that over half of respondents were ‘somewhat or very concerned about mpox in their community.’ Another point of research in the survey found that 32% of respondents listed social media as their source of information, followed by 30% who listed a health care provider.
Dr. Holloway, who is also a professor of social welfare at UCLA, said that community input is essential in creating and improving public health strategies to combat mpox infections and raise awareness about the effectiveness of vaccinations.
This survey was done as a partnership between the research center and StickItin.LA.
“Through StickItIn.LA, we’re creating a platform to listen and connect to those who’ve been directly impacted by mpox and by doing so, we can shape a more inclusive vaccination strategy that addresses both stigma and mistrust,” said Dr. Holloway.
Human health studies & sciences
Sexually transmitted hard-to-treat fungal skin infections now in U.S.
This sexually transmitted form of ringworm has been increasingly diagnosed throughout Europe, reported mostly in men who have sex with men

NEW YORK – Healthcare providers should watch out for new and highly contagious forms of ringworm or jock itch, which are emerging as a potential public health threat, according to a pair of reports.
In the first of the studies, experts at NYU Langone Health who focus on the spread of contagious rashes document the first reported case in the United States of a sexually transmitted fungal infection that can take months to clear up, even with treatment. In the second report, NYU Langone physicians partnered with authorities at the New York State Department of Health to describe the largest group of patients in the country with a similar fungal strain that resists standard therapies.
Both species of fungi are among a group that causes skin rashes, or tinea, which easily spread on the face and limbs (ringworm), groin (jock itch), and feet (athlete’s foot). However, the tinea explored in the new reports can look very different from the neat, regular circles seen in most forms of ringworm. They may instead be confused for lesions caused by eczema and can therefore go without proper treatment for months.

The first report, which published online on June 5 in the journal JAMA Dermatology, describes a man in his 30s who developed tinea on his penis, buttocks, and limbs after returning home to New York City from a trip to England, Greece, and California. Genetic tests of fungal samples collected from the patient’s rashes revealed that the infection was caused by the species Trichophyton mentagrophytes type VII (TMVII).
This sexually transmitted form of ringworm has been increasingly diagnosed throughout Europe, with 13 instances reported in France in 2023, mostly in men who have sex with men. Notably, the man in the current study said he had sex with multiple male partners during his travels, none of whom reported similar skin issues.
“Healthcare providers should be aware that Trichophyton mentagrophytes type VII is the latest in a group of severe skin infections to have now reached the United States,” said study lead author and dermatologist Avrom S. Caplan, MD. Dr. Caplan is an assistant professor in the Ronald O. Perelman Department of Dermatology at NYU Grossman School of Medicine.
“Since patients are often reluctant to discuss genital problems, physicians need to directly ask about rashes around the groin and buttocks, especially for those who are sexually active, have recently traveled abroad, and report itchy areas elsewhere on the body,” added study senior author John G. Zampella, MD.

(Photo Credit: JAMA Dermatology)
Dr. Zampella, an associate professor in the Ronald O. Perelman Department of Dermatology, says that while infections caused by TMVII are difficult to treat and can take months to clear up, they so far appear to respond to standard antifungal therapies, such as terbinafine.
Meanwhile, Dr. Caplan says the new skin condition explored in his other new report presents a greater challenge for dermatologists. The study results, published online in May in JAMA Dermatology, center on Trichophyton indotineae, which is widespread in India and is now reported globally. First confirmed in the United States last year, the infection causes itchy and contagious rashes similar to those of TMVII, but it often resists terbinafine treatment.
To better understand how T. indotineae can evade antifungal drugs, the researchers collected clinical and laboratory data from 11 men and women treated for ringworm in New York City hospitals between May 2022 and May 2023. Their tinea was confirmed to have been caused by T. indotineae. Seven of the patients had received standard doses of terbinafine for anywhere from 14 days (the usual duration for most forms of ringworm) to 42 days, yet their rashes did not improve.
Analyzing the fungal samples’ DNA, the team reported several variations in the genetic code (mutations) that prevent terbinafine from hooking onto fungal cells and poking holes in their protective membranes. According to the study authors, these mutations might help explain why the therapy often failed in some cases to fight the infections.
The results also showed that when seven patients were treated with another antifungal called itraconazole, three recovered entirely and two improved. The problem with this therapy, Dr. Caplan says, is that while effective, the drug can interfere with many medications and can cause nausea, diarrhea, and other side effects that make it hard to use for long periods.
“These findings offer new insight into how some of the fungal skin infections spreading from South Asia can evade our go-to therapies,” said Dr. Caplan. “Beyond learning to recognize their misleading signs, physicians will need to ensure their treatment addresses each patient’s quality of life needs.”
Dr. Caplan adds that he plans to work with leading fungi experts around the United States and internationally over the next few months to expand research efforts and track emerging cases.
The researchers caution that while dermatologists should be on the alert for signs of TMVII and T. indotineae in their patients, rates so far remain low in the United States.
Study funding was provided by NYU Langone.
-

 Commentary2 days ago
Commentary2 days agoThe perfect storm: Our queer infrastructure is in crisis
-
 a&e features4 days ago
a&e features4 days agoUltimate guide to queer gift giving
-

 a&e features3 days ago
a&e features3 days ago“I should have been there”: A queer Korean adoptee finds healing with original family members
-
 Books5 days ago
Books5 days ago‘90s club kids will love Mark Ronson’s new book
-

 California3 days ago
California3 days agoRicardo Lara, John Heilman inducted into Victory Institute’s Hall of Fame
-

 Golden Globe Awards4 days ago
Golden Globe Awards4 days agoCynthia Erivo, Eva Victor, and ‘Blue Moon’ bring queer representation to Golden Globe film nominations
-

 LGBTQ+ Youth Mental Health2 days ago
LGBTQ+ Youth Mental Health2 days agoL.A. County officials advocate to reinstate “Press 3” crisis hotline for young queer people
-

 Television23 hours ago
Television23 hours ago‘Heated Rivalry’ is the gay hockey romance you didn’t know you needed
-

 Commentary14 hours ago
Commentary14 hours agoLove in the time of porn: a glimpse into the dating life of an adult performer